You choose the cover to suit your budget and lifestyle - 60 75 or 90 back from Members Choice providers. In general Medicare doesnt cover blood pressure monitors also known as ambulatory blood pressure monitoring devices for use at home.
 How Does Health Insurance Work In The Netherlands Student Guide
How Does Health Insurance Work In The Netherlands Student Guide
Insurance does not typically cover blood pressure monitoring kits but be sure to contact your insurance company with questions about coverage options.

Does insurance cover blood pressure monitor. Your insurance covers the cost of the monitor. If you regularly need to monitor your blood pressure at home blood pressure monitors may be covered by your private health insurance. Medicare coverage for home blood pressure monitors is available under certain conditions.
In some scenarios Medicare will pay for the temporary use of a different kind of blood pressure device called an ambulatory blood pressure monitor. ABPM is a non-invasive diagnostic test that uses a device to track blood pressure over 24-hour cycles allowing a doctor to assess a patients blood pressure during routine daily living instead of when they are sitting nervously on an. An ABPM is a non-invasive monitor that measures your blood pressure in 24-hour cycles and stores the measurements in the device.
Stress smoking eating exercise cold pain noise medicines and even talking can affect it. Most people use an automatic monitor to measure their blood pressure at home. 052020 - The purpose of this change request is to inform contractors that for dates of service on and after July 2 2019 CMS will cover Ambulatory Blood Pressure Monitoring for the diagnosis of hypertension in Medicare beneficiaries under updated criteria.
Purchase a monitor at your local pharmacy. The cost of a monitor is 40-100 depend-ing on size. Cover for a wide range of services including more costly ones like major dental orthodontics and hearing aids.
Your monitor might have a feature that will record your numbers for you. Cardiovascular Health Assessment. Automatic blood pressure monitors.
Many insurance companies do not pay for blood pressure monitors. The cuff wraps around your upper arm. It does not cover regular cuff blood pressure monitors except for people undergoing dialysis at home.
Today the Centers for Medicare Medicaid Services CMS finalized its national coverage policy for Ambulatory Blood Pressure Monitoring ABPM. Medicare will cover the use of the device once a year per patient. What is an ambulatory blood pressure monitor ABPM.
Coverage is available when blood pressure checks are carried out by a. When you press the start button on the monitor. Medicare may also help cover a blood pressure monitor.
If this is the case Medicare will provide a blood pressure cuff and a stethoscope to allow for blood pressure and heart rate monitoring during treatment. You are undergoing renal dialysis at home Your doctor recommends an ambulatory blood monitoring device ABPM. Someone with a systolic pressure of 120 and a diastolic pressure of 80 has a blood pressure of 12080 or 120 over 80 Blood pressure is measured in millimeters of mercury mm Hg.
The exception is if you have suspected white coat syndrome a condition where a patient has an above-normal blood pressure reading in a clinical environment but not in other situations. These are also called electronic or digital monitors. Medicare may provide coverage for a blood pressure monitor at home if you are receiving dialysis treatments at home.
If your insurance does not cover the cost these are some options. Medicare does not cover the cost of a blood pressure monitor for use at home. Record your blood pressure numbers with the date and time.
Medicare generally does not pay for at-home blood pressure monitors except in certain circumstances. This type of purchase often qualifies for reimbursement through a patients flexible spending account or health savings account. 100 back on up to two dental check-ups every year including bitewing x-rays at any Members Choice Advantage dentist 1 OR.
Your high blood pressure is not under control You have been taking your tablets for less than three months. Travel Insurance Cover and High Blood Pressure The insurer may not cover you for any risks linked to high blood pressure if. Updated on April 6 2021.
To have cover for blood pressure monitors you will generally need to have a comprehensive extras policy. You might use a home blood pressure log or a spreadsheet on your computer. Medicare Part B may pay for you to rent an ambulatory blood pressure monitor once a.
As part of this program youre eligible to receive a new blood pressure monitor every two years. The devices called ambulatory blood pressure monitoring is helpful for clinicians with patients who are nervous in clinical. As a member you also have access to a variety of WebMD tools and resources that help you manage monitor and understand your condition.
Medicare insurance does not generally provide coverage for blood pressure monitors for use in the home unless you meet specific criteria. They have a microphone to detect blood pulsing in the artery. Medicare covers a device called an ambulatory blood pressure monitor for use once a year when ordered by a doctor.
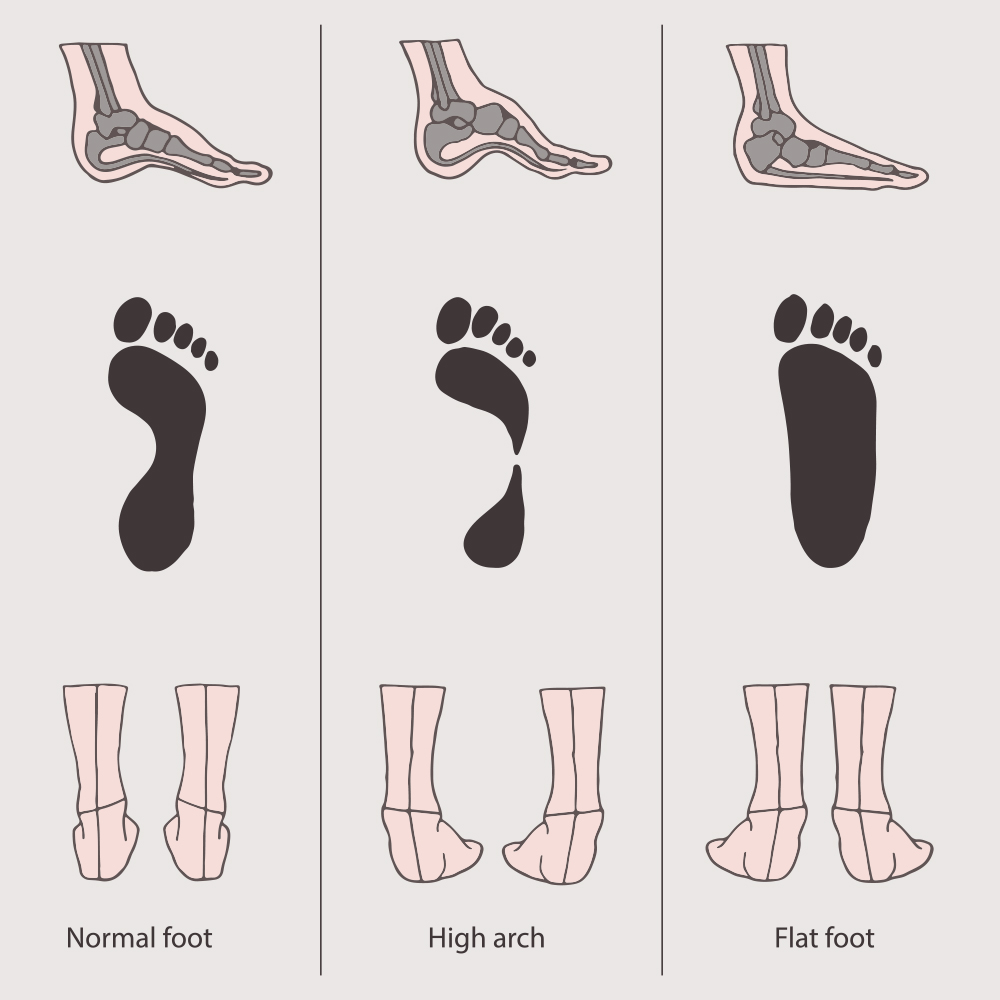
Check your policy to see if youre covered for health appliances and health monitoring equipment. We do not recommend the wrist. Blood pressure tends to be higher in the morning and lower at night.
Medicare Part B medical insurance may sometimes cover blood pressure monitors if. Lifesource and Omron are reliable brands. For example if youre undergoing home kidney dialysis.