Eucrisa Crisaborole Topical Generic Name. Selected from data included with permission and copyrighted by First Databank Inc.
 Eczema Treatment Eucrisa Crisaborole Safety Info
Eczema Treatment Eucrisa Crisaborole Safety Info
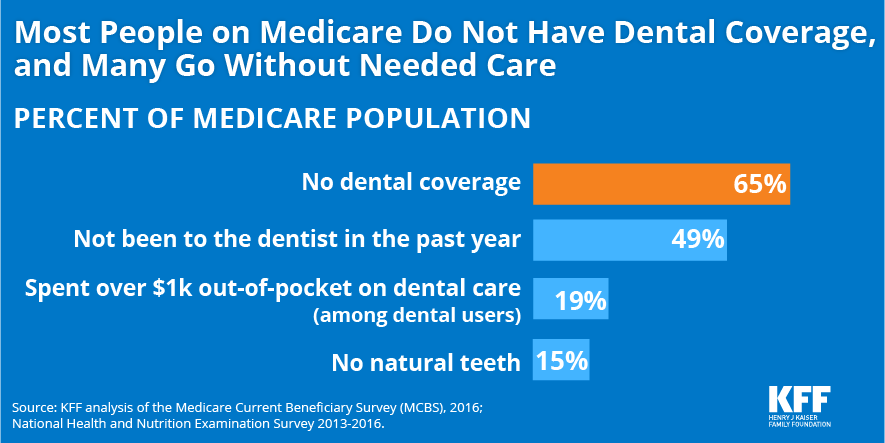
Does my states Medicaid program cover CGM.
Does medicaid cover eucrisa. Mandatory benefits include services including inpatient and outpatient hospital services physician services laboratory and x-ray services and home health services among others. Eucrisa 2 60 gm or 100 gm tube 1 tube per 30 days Hypersensitivity reactions including contact urticarial have occurred. 1-16 of 75 results for eucrisa Eucerin Creme Eczema Relief Hand 27 Ounce Tube 80ml 3 Pack 49 out of 5 stars 14.
Severe pruritus swelling or erythema at the application site or distant site may be indicative of hypersensitivity. Crisaborole topical for use on the skin is used to treat mild to. As Medicaid access expands so does cancer survival More lower-income Americans are surviving cancer due to expanded Medicaid health care coverage a new study shows.
Use of EUCRISA in this age group is supported by data from two 28-day adequate vehicle-controlled safety and efficacy trials which included 1313 pediatric subjects ages 2 years to 17 years of whom 874 received EUCRISA. This drug will likely be quite expensive and you may want to consider using a GoodRx discount instead of Medicare to find the best price for this prescription. The most commonly reported adverse reaction in subjects 2 years and older was application site pain.
For Atopic Dermatitis. In general Medicare plans do not cover this drug. For example some states only cover CGM for type 1 diabetes and other states have differing policies for short-term and long-term CGM use.
Used the entire tube. Unfortunately Medicare doesnt typically cover absorbent products. More Buying Choices 2448 6 new offers Eucerin Baby Eczema Relief Body Cream - Steroid Fragrance Free for 3 Months of Age - 5 Oz Tube.
Patients currently on Eucrisa therapy as documented in claims history will be allowed to continue on their current therapy. Paid 30 after insurance coverage but its not effective for my issue. Medicaid does cover for orthotics but that coverage will vary from state to state.
Eucrisa medication page for healthcare professionals to search for scientific information on Pfizer medications. Eucrisa crisaborole topical is a member of the miscellaneous topical agents drug class and is commonly used for Atopic Dermatitis. Yes No Positive clinical response to EUCRISA therapy eg reduction in body surface area involvement reduction in pruritus severity etc Quantity Limit.
Continued for 2 weeks its worse. However Medicare may cover non-absorbent products such as catheters and related products. Optional benefits include services including prescription drugs case management physical therapy and.
Eucrisa Prices The cost for Eucrisa topical ointment 2 is around 711 for a supply of 60 grams depending on the pharmacy you visit. This document contains c onfidential and proprietary information of CVS Caremark and cannot be reproduced distributed or printed without written permission from CVS Caremark. In order to obtain coverage for these products youll need to obtain a physicians order or a prescription stating what is needed for treating your incontinence.
Medicaid is a joint Federal-State program that pays for medical assistance for individuals and families with low incomes and relatively few assets. Also find the prescibing information announcements resources and channels to connect with Pfizer Medical Information. Topical Immunomodulators Eucrisa TX Medicaid C10818A 06- -2017doc 2017 CVS Caremark.
This survey is being conducted by the WebMD marketing sciences department. Although pharmacy coverage is an optional benefit under federal Medicaid law all states currently provide coverage for outpatient prescription drugs to all categorically eligible individuals and most other enrollees within their state Medicaid programs. More bumps rash and itching.
In some instances if you have Medicare as well Part B could cover orthotic devices or braces to support weak joints or muscles. For patients with claims history documenting prior use of either topical corticosteroids or topical calcineurin inhibitors a prescription for Eucrisa will automatically process. It appeared to have worked after 2-3 days but then the breakouts got worse.
Even if CGM is covered under your states policy each state has its own criteria for which individuals qualify to receive it. How much is my Eucrisa co-pay with Medicare. After being diagnosed with a topical dermatitis I was prescribed Eucrisa.
47 849Count FREE Shipping. Only 6 left in stock - order soon. This copyrighted material.