61 To report SUSPECTED ADVERSE REACTIONS contact Astellas Pharma US Inc. You are now leaving the site and connecting to an outside source.
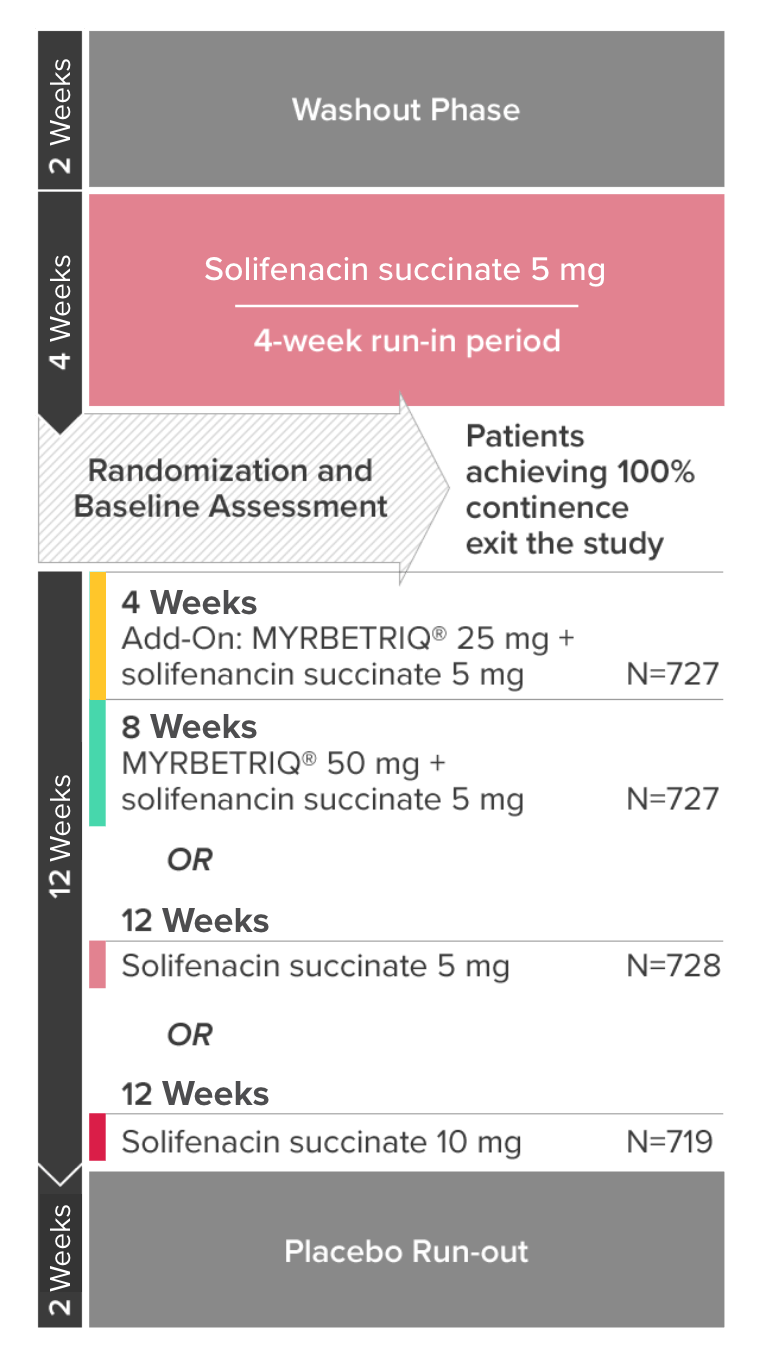
 Efficacy And Safety Of Mirabegron Add On Therapy To Solifenacin In Incontinent Overactive Bladder Patients With An Inadequate Response To Initial 4 Week Solifenacin Monotherapy A Randomised Double Blind Multicentre Phase 3b Study Beside
Efficacy And Safety Of Mirabegron Add On Therapy To Solifenacin In Incontinent Overactive Bladder Patients With An Inadequate Response To Initial 4 Week Solifenacin Monotherapy A Randomised Double Blind Multicentre Phase 3b Study Beside
Office Address Line 1 required PO boxes not accepted City required State required Zip required.
Myrbetriq sample request form. We are available MondayFriday 900 am 800 pm ET. Myrbetriq mirabegron a beta-3 adrenergic agonist is indicated as monotherapy or in combination with the muscarinic antagonist solifenacin succinate for the treatment of overactive bladder OAB with symptoms of urge urinary incontinence urgency and urinary. Microsoft Forms automatically provides charts to visualize your data as you collect responses in real time.
800-477-6472 or Visit website. By signing this form I request the drug samples listed herein and certify that I am a licensed practitioner currently authorized under applicable federal and state law to request receive and dispense these drug samples. By completing the form below you will receive samples for.
At 1 -800-727-7003 or FDA at 1 -800-FDA-1088 or wwwfdagovmedwatch. 08222018 CAT0295 Page 3 of 3 11719 FAX THIS FORM TO. Healthcare providers may request samples for their practice by logging onto the website.
800-424-7640 2017 2018 Magellan Health Inc. We oversee programs for over-the-counter and prescription products including controlled substances. How to request samples vouchers andor coupons.
I also certify that I have requested these samples for the legitimate medical needs of my patients. LIVALO 4 mgSix sample packs containing 7 tabletseach. Myrbetriq Support Solutions provides information regarding patient healthcare coverage options and financial assistance options that may be available to help patients with financial needs.
----- DRUG INTERACTIONS -----. You may also call 88861AVION 18886128466 to request free samples. Quickly create quizzes to measure student knowledge evaluate class progress and focus on subjects that need improvement.
This site is intended to allow licensed health care practitioners the ability to order samples of prescription drugs. Easily create surveys and polls to collect customer feedback measure employee satisfaction and organize team events. Myrbetriq mirabegron a beta-3 adrenergic agonist is indicated as monotherapy or in combination with the muscarinic antagonist solifenacin succinate for the treatment of overactive bladder OAB with symptoms of urge urinary incontinence urgency and urinary frequency.
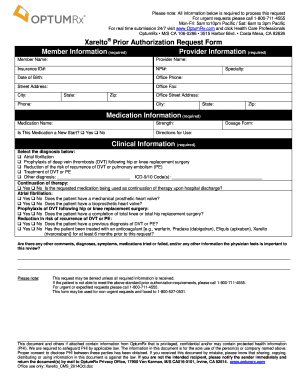
Myrbetriq mirabegron Prior Authorization Request Form Caterpillar Prescription Drug Benefit Phone. To speak with a dedicated access specialist please call us at 1-800-477-6472. Reference Practitioners Last Name required First Name required Professional Designation - Select One required MD DO NP PA.
Request Samples of LIVALO. To request samples vouchers andor coupons please log in to eMedSample or register using your last name and NPI national provider identifier number. Please allow 7 to 10 businessdays for delivery.
SAMPLE REQUEST FAX FORM Fax to 973-644-2386. Our FDA and PDMA-compliant systems allow clients to maintain a high level of sampling activity with the. Any data you choose to provide to Physicians Interactive will be governed by SymmetryRx Privacy Policy.
SAMPLE Letter of Appeal For Myrbetriq mirabegron extended-release tablets Date Payer Name Payer Address City State ZIP Code Payer Fax Number Attn. All of the relevant parameters will be analysed and you will receive by mail a detailed evaluation as well as recommendations on how to improve the water quality. Request a sample bottle from us then fill it with water from your pond and send it to our lab in the box with our address on it.
Myrbetriq is not for everyone. Do not take Myrbetriq if you have an allergy to mirabegron or any ingredients in Myrbetriq. Myrbetriq Number of uses.
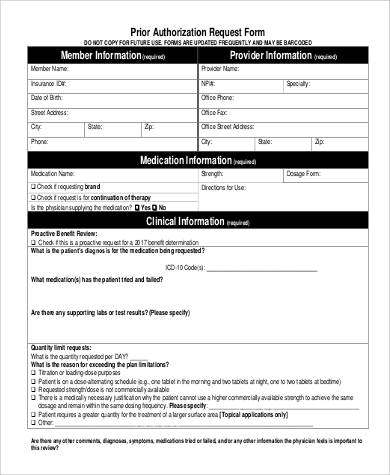
Payer Representative Department Name optional Fill Sign Online Print Email Fax or Download. MySampleCloset is a website built and maintained by J. Do not take MYRBETRIQ if you are allergic to mirabegron or any ingredients in MYRBETRIQ.
If you are a healthcare professional and would like to receive samples of Prenate products for your patients please fill out the sample request form below. Myrbetriq mirabegron is a prescription medicine for adults used to treat overactive bladder OAB with symptoms of urgency frequency and leakage. MYRBETRIQ mirabegron extended-release tablets is a prescription medicine for adults used to treat overactive bladder OAB with symptoms of urgency frequency and leakage.
Form more information phone. License numbers and addresses will be verified prior to shipping. Magellan Rx Management Commercial Clients.
I understand that the sale or offer to sell a drug. Samples are available to prescribers only. To receive your samples of Osphena ospemifene tablets 60mg.
LIVALO 2 mgSix sample packs containing 7 tabletseach. MYRBETRIQMYRBETRIQ Granules in pediatric patients with NDO 3 were UTI nasopharyngitis constipation and headache. You can also downloadand fax the form.