View Profile View Forum Posts Private Message View Blog Entries View Articles Senior Member Funding. Street Address Street Address City State and Zip This notice contains important information about your right to continue your health care coverage in the ABC Company Group Health Plan the Plan.
The advanced tools of the editor will lead you through the editable PDF template.
How to fill out cobra form. Sample COBRA Notice ABC Company co The COBRA Administrators Name 1234 South St City State and Zip 06102008 PQB Name. I did go down and get gas and fill the Coupe up yesterday so it will be ready when I am. Level was an inch below reading on the dip stick.
The advanced tools of the editor will guide you through the editable PDF template. Read the post on filling correctly for the cobra. Right after buying templates users can find them in the My Forms section.
Print and send completed form. The individual then has 60 days to decide whether to elect COBRA continuation coverage. Tips on how to complete the Get And Sign Cobra Enrollment Form 2011-2019 on the web.
Find a suitable template on the Internet. The Physicians Authorization for Transfer form Attachment A for transfer is completed. If an employee or dependent chooses to elect COBRA the employee or dependent can request special enrollment in another group health plan or the Marketplace once COBRA is exhausted.
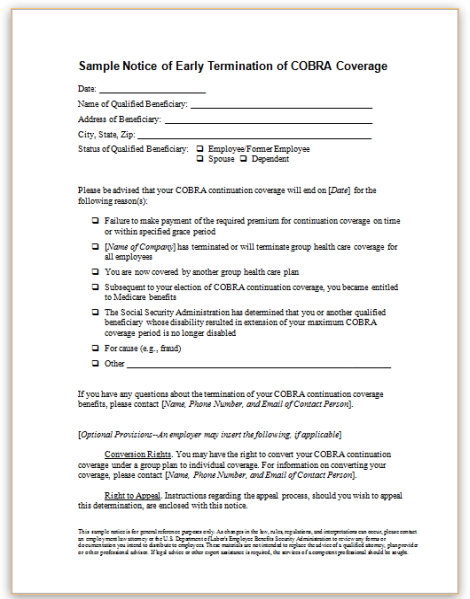
For instructions see Fill out your PDF form. In order to exhaust COBRA coverage the individual must receive the maximum period of COBRA coverage available without early termination. To download a template from US Legal Forms users simply need to sign up for a free account first.
Termination Request Form Live Chat. Incomplete incorrect andor illegible forms will be returned back to the sender and require a new form submission. To obtain a US Legal Forms subscription online follow the guidelines below.
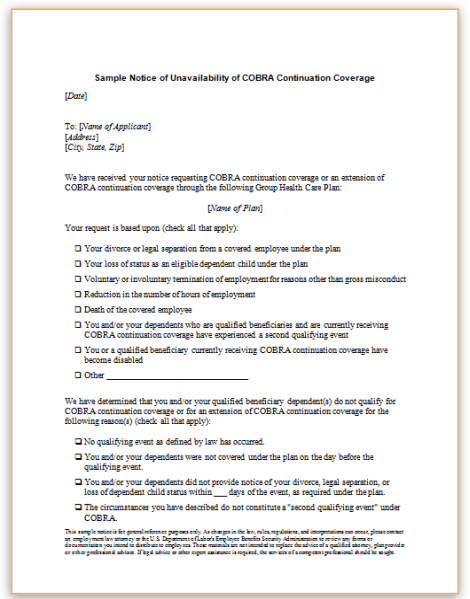
Video instructions and help with filling out and completing Cobra Election Form For Employee To SignForm. Use of the model general notice appropriately completed will be considered by the Department to be good faith compliance with the general notice content requirements of COBRA. If you are satisfied fill out and return the election form within the election period to enroll in COBRA coverage.
To use this model election notice properly the Plan Administrator must fill in the blanks with the appropriate plan information. To begin the document utilize the Fill Sign Online button or tick the preview image of the form. In 310 the build isnt changed a lot as it hasnt been affected much by the balance changes.
In order to use this model general notice properly the plan administrator must complete it by filling in the blanks with the appropriate plan information. Enter your official identification and. Tips on how to fill out the Cobra election form 2013-2019 on the web.
The Department considers use of the model election notice to be good faith compliance with the election notice content requirements of COBRA. The acknowledgement of the notification of the transfer by the patient or the legal. In the meantime people can fill out a form available on the departments website submitting to the main eligibility requirements.
07-10-2020 0610 AM 7. Cobra Lash Poison Assassin Version Notice Ive created this guide in 38 and updated it for 39 and now 310. The advanced tools of the editor will lead you through the editable PDF template.
Read all the field labels carefully. To start the document utilize the Fill Sign Online button or tick the preview image of the document. That they had a qualifying event such as job loss or a reduction in hours and are not eligible for Medicare or another group health plan.
Could not get dipstick out so removed cover. If you are already registered on our service log in and select the document you need and purchase it. Save form open in Acrobat or Acrobat Reader and then choose Tools Fill Sign.
Additional information about signing up for COBRA is included in the Summary Plan Description provided by the employer at the start of your coverage. Start filling out the blanks according to the instructions. It is very darkalmost black.
The Department of Labor has developed a model Consolidated Omnibus Budget Reconciliation Act of 1985 COBRA continuation coverage election notice that the Plan may use to provide the election notice. PO Box 3938 Manchester NH 03105 Please completely fill out this form to request for COBRA Termination. This notice must be sent to the plan participants and beneficiaries by first class mail or hand delivered not later than 14 days after the plan administrator receives notice that a qualifying event occurred.
It has finally cooled down to around the 101108 mark but that is still to much heat for me to enjoy being out in it. If the form does not contain interactive fields you can use the Fill Sign tools to fill out the form. Enter your official identification and contact details.
Wanted to check the level on a boat I just bought. To begin the document utilize the Fill Sign Online button or tick the preview image of the form. The nerf to precision however made me remove it from the setup.
Previous owner said changed this 2 weeks ago during winterizing. Enter your official contact and. The patient may be transferred upon completion of the COBRA Transfer Checklist and Patient Transfer Summary Attachment C.
An individual must request. Save the form on your computer and then open it directly in Acrobat or Acrobat Reader. How to fill out the Cobra election form on the internet.
To start the blank utilize the Fill Sign Online button or tick the preview image of the form. The way to fill out the Paychex cobra form employee data sheet employee data sheet form on the web. The advanced tools of the editor will lead you through the editable PDF template.