Medicare Advantage MA plans also often require prior. Call 1-800-711-4555 5 am.
 Free Medicare Prior Rx Authorization Form Pdf Eforms
Free Medicare Prior Rx Authorization Form Pdf Eforms
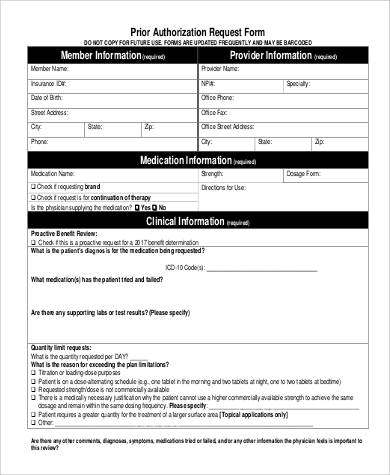
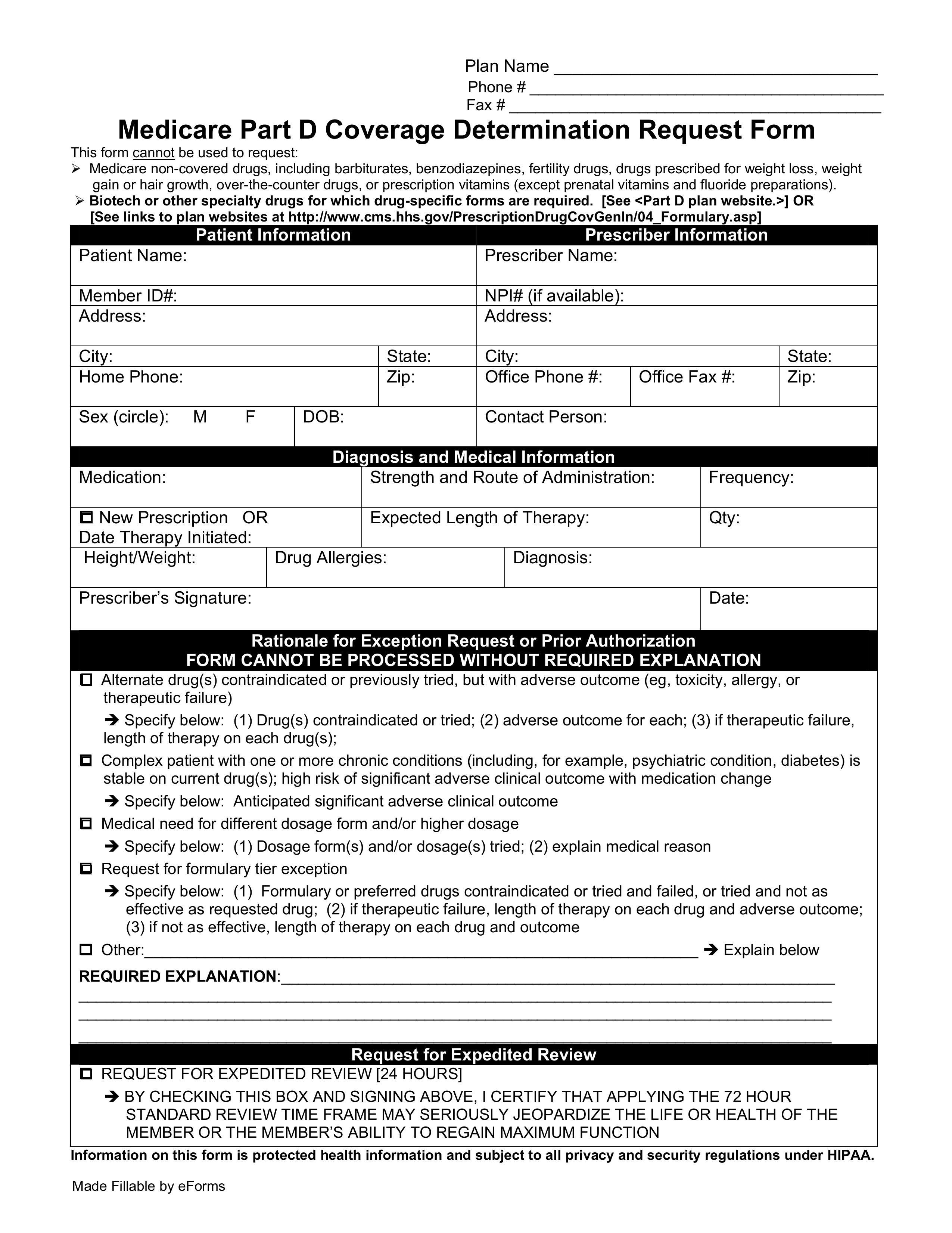
If the prescribed medication requires a Prior Authorization you can request a Coverage Determination Request asking the plan to review the request to approve coverage of the medication.

Medicare part d prior authorization phone number. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. Prior authorization is the process of receiving written approval from WPS for services or products prior to being rendered. 1-800-523-0023 Changes to your contract information Participating physicians hospitals facilities and other healthcare providers are asked to update their service address and other contact information address phonefax numbers etc promptly when changes occur.
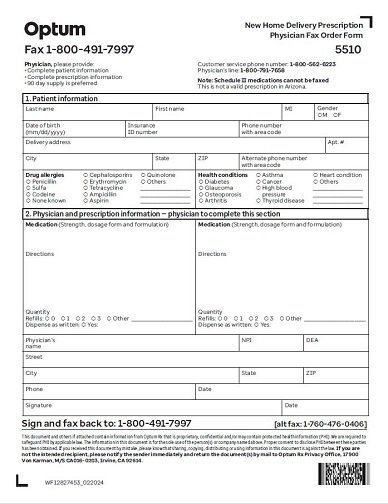
PT Monday-Friday and 6 am. All Medicare authorization requests can be submitted using our general authorization form. You can submit a verbal PA request.
Other ways to submit a prior authorization Having difficulties with ePA. 8 pm local time. You can find the number for Member Services on your plans member ID card.
Please check back as we will continue to update these resources regularly. Click on the contact list that best matches your information needs. May not result in near real-time decisions for all prior authorization types and reasons.
TTY users call 18007163231. Whose responsibility is it. Express Scripts manages prior authorizations and Non-Formulary requests for Medicare Part D prescriptions.
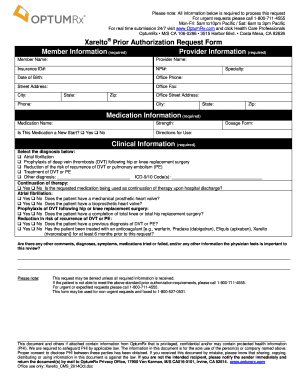
We encourage customers to verify prior authorization. Medications that require prior authorization. View Part D prior authorization requirements.
PT Saturday If you cannot submit requests to the OptumRx PA department through ePA or telephone click here. Contact CVS Caremark Prior Authorization Department Medicare Part D. Private for-profit plans often require Prior Authorization.
The provider requests and submits the prior authorization. This page contains contact information for specific contacts at Part D sponsors. Prior authorization is a requirement that a health care provider obtain approval from Medicare to provide a given service.
The following information is generally required for all authorizations. Submit online at Express Scripts or call 1-800-935-6103. If you want Medicare to be able to give your personal information to someone other than you you need to fill out an Authorization to Disclose Personal.
1-800-MEDICARE 1-800-633-4227 For specific billing questions and questions about your claims medical records or expenses log into your secure Medicare account or call us at 1-800-MEDICARE. 1-800-711-4555 option 2 If you are having a medical crisis please call 911 or contact your. Prior authorization or exception request.
Prior Authorization is about cost-savings not care. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. What is Prior Authorization.
If you are unable to use electronic prior authorization you can call us at 1 800 882-4462 to submit a prior authorization request. Your doctor can help you correctly complete the form. Step 3 Under Prescriber Information enter the physicians name NPI number address phone number fax number and contact person.
Fax the request form to 8886476152. Medicare Part D Medications. Step 2 In the Patient Information section provide the patients name ID number address phone number gender and date of birth.
Submitting an Authorization Request. Under Prior Authorization benefits are only paid if the medical care has been pre-approved by Medicare. Call 18664775703 24 hours a day 7 days a week except Thanksgiving and Christmas.
Part D Contacts. For medical service preauthorization requests and notification. The online option is a useful way to print the documents and take them to your doctor.
Call 1-800-555-CLIN 2546 Monday Friday 8 am. Medicare Advantage Prior Authorization. The fastest and most efficient way to request an authorization is through our secure Provider Portal however you may also request an authorization via fax or phone emergent or urgent authorizations only.
Retiring Admission Notification Fax Numbers. Services are still subject to all plan provisions including but not limited to medical necessity and plan exclusions. Also recipients may directly contact their Part D plan and ask for a mail-in form.
Most Part D plans have forms you can download online. Prior authorization medications require the plans approval before the medication will be covered. In this section you will find the tools and resources you need to help manage your practices prior authorization and notification requirements with program specific information available for Cardiology Oncology Radiology Clinical Pharmacy and Specialty Drugs.