Walgreens Custodian of Records 1901 East Voorhees St MS 735 Danville Illinois 61834. PRESCRIBER INFORMATI ON Prescribers name.
 Walgreens Custodian Of Records Fill Out And Sign Printable Pdf Template Signnow
Walgreens Custodian Of Records Fill Out And Sign Printable Pdf Template Signnow
Safe on-time delivery of medications if available Patient Bill of Rights.

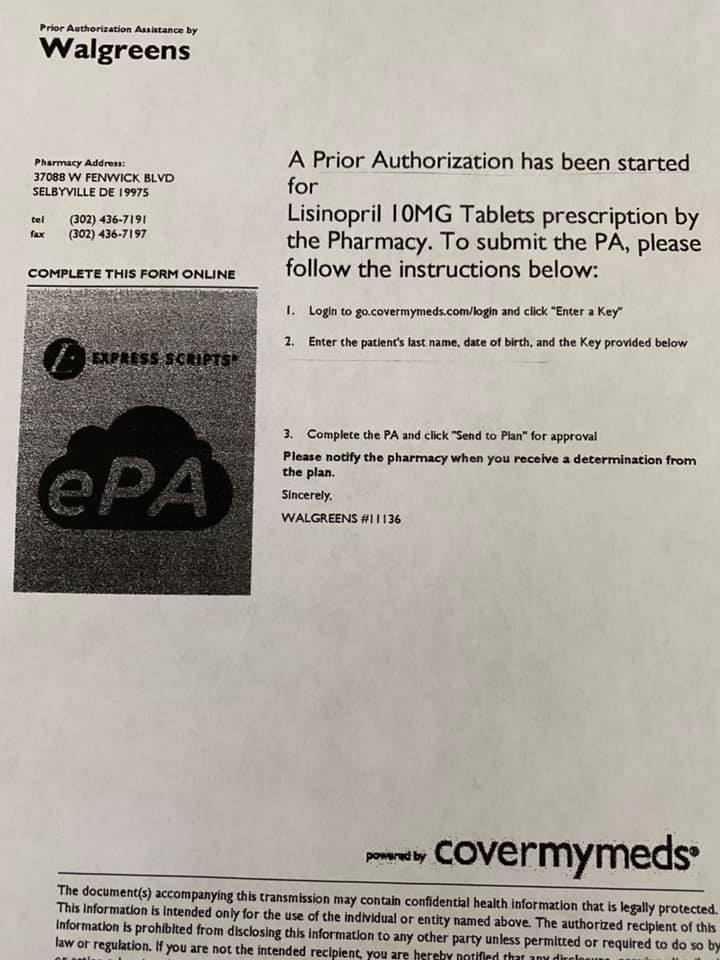
Walgreens prior authorization. Prior Authorization is a term used for select services eg homecare services items eg Durable Medical Equipment purchases over 500 and prescriptions for some injectable or infusion drugs eg Botox Soliris OxyContin that must be pre-approved by Health Partners Plans. Insurance verification and help with prior authorization. Authorization for supplies runs concurrently with the number of refills or time frame specified for th e drug.
I certify that the clinical information provided on this form is complete and accurate. Walgreens Pharmacy Services allow you to conveniently fill prescriptions chat with a pharmacist set reminders and more. We put our hearts into connecting you and your patients to the people organizations and services that can make a meaningful difference.
Find a Walgreens store near you. If faxed the fax must come from MD office or hospital should not be faxed by patient. Prior Authorizations are sometimes referred to as preauthorizations or.
Prior authorization is a restriction put in place by insurance companies so they can decide whether or not they will pay for certain medicines. The Massachusetts Supreme Judicial Court wrote that Walgreens had a limited duty to take reasonable steps to notify both Rivera and her doctor of the need for prior authorization each time. If you dont get approval the plan may not cover the drug.
Then select the Prior Authorization and Notification tool on your Link dashboard. Walgreen Company dba Walgreens. Delivery Pickup Options - 2 reviews of Walgreens The prescription I dropped off required a prior authorization from my doctor.
To request prior authorization please submit your request online or by phone. Financial assistance support when available. The plan requires you or your doctor to get prior authorization for certain drugs.
Contact Walgreens Pharmacy today. Usually just an additional form. Use the Prior Authorization and Notification tool on Link.
Central specialty medications are now filled by AllianceRx Walgreens Prime a combined. Specialty Pharmacy Welcome Booklet Espanol. This means the plan needs more information from your doctor to make sure the drug is being used correctly for a medical condition covered by Medicare.
It doesnt affect cash payment for prescriptions and its only required on those prescriptions when billed through insurance so if youre uninsured or if you decide to pay in cash you wont need to worry about getting prior. Parent or guardian if minor First name. This wouldnt be a problem if they faxed over the prior auth form to my doctor.
Explain your authority to act see instructions for additional information that may be required Section 9. Rein was a pharmacist store manager district manager and treasurer prior to being named Chief Executive Officer and Chairman of the Board. Side effect management and adherence support.
See details on the specialty pharmacy services medications and expert care Walgreens offers. 1 Our passion is personal. Donate to Red Nose Day.
Certain Drugs require you or your doctor to get prior authorization in order to be covered. On October 10 2008 Rein abruptly quit as CEO and was replaced by Alan. Please call us at 8007532851 to submit a verbal prior authorization request if you are unable to use Electronic Prior Authorization.
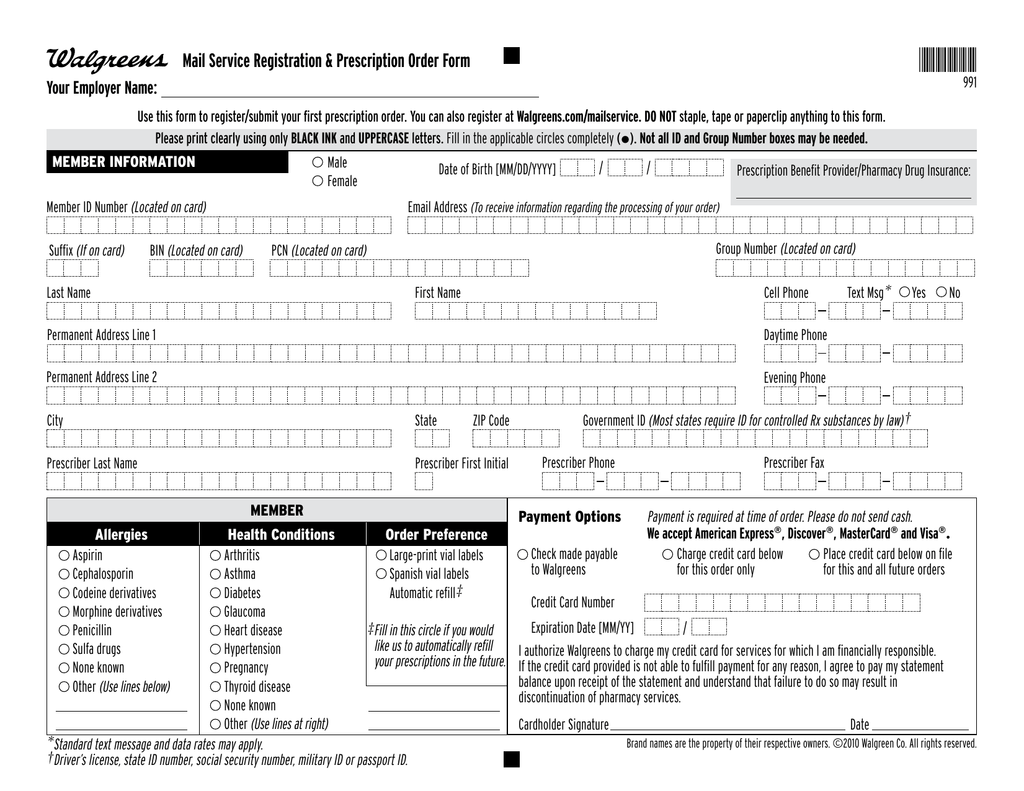
Mail this completed and signed form to. This form is intended for prescriber use only. We helped connect eligible specialty patients to more than 490 million in financial assistance in 2018.
Walgreens or its affiliates may contact you including by autodialed and prerecorded calls and texts at any time using the contact information provided in your patient record regarding health and safety matters such as vaccine reminders. Greg Wasson former President of Walgreens Health Services was named President and Chief Operations Officer. Supporting progress notesclinical documentation are attached - failure to attach may result in delay.
Attestations required for prior authorization review. If your prescribing doctor feels it is necessary to exceed the set limit he or she must get prior approval before the higher quantity will be covered. For Internal Use Only Approved.
Aside from receiving a text message that my medication was being delayed the pharmacy never notified me the medication needed approval. If you cant submit a request via telephone please use our general request form or one of the state specific forms below and fax it.
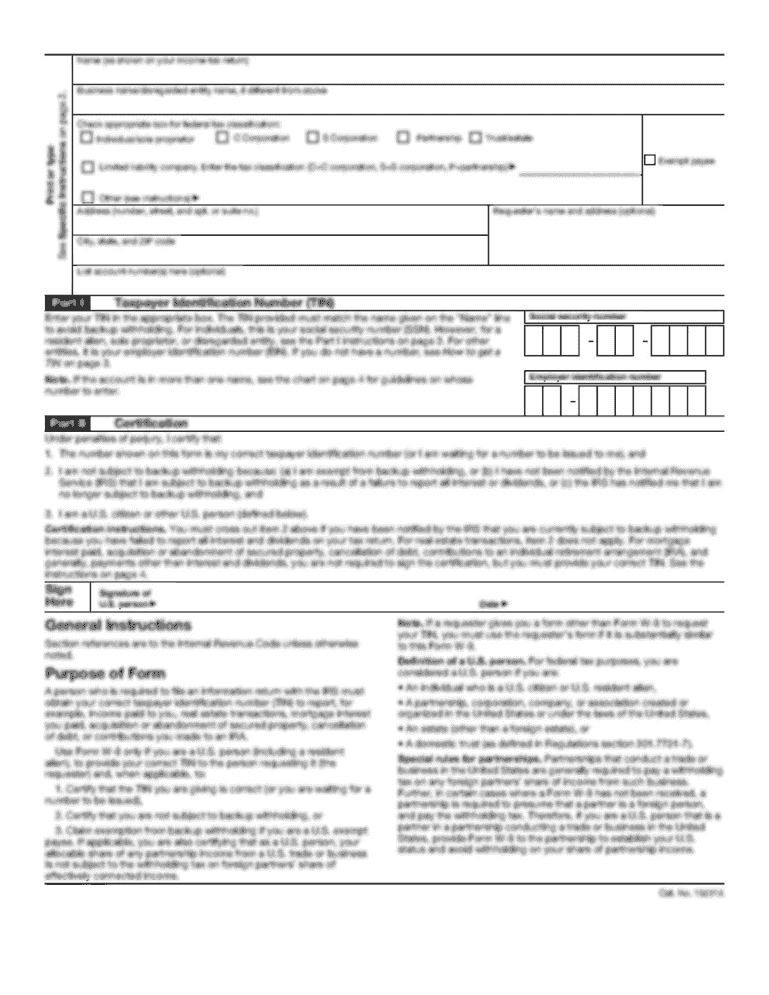 Walgreens Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Walgreens Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
 Walgreens Application Fill Online Printable Fillable Blank Pdffiller
Walgreens Application Fill Online Printable Fillable Blank Pdffiller
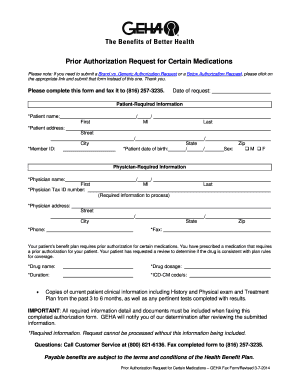 Geha Pre Authorization Form Fill Online Printable Fillable Blank Pdffiller
Geha Pre Authorization Form Fill Online Printable Fillable Blank Pdffiller
 Fillable Online Walgreens Medmark Orthopedic Prescription Pharmacy Intake Form Fax Email Print Pdffiller
Fillable Online Walgreens Medmark Orthopedic Prescription Pharmacy Intake Form Fax Email Print Pdffiller
 And The Bullsh T Prior Authorizations Keep Coming Authentic Medicine
And The Bullsh T Prior Authorizations Keep Coming Authentic Medicine
 Mommydoc Prior Authorizations Who Is Responsible For The Death Of A Patient When Insurers Practice Medicine
Mommydoc Prior Authorizations Who Is Responsible For The Death Of A Patient When Insurers Practice Medicine
Seeking Clarification About Wag Medicare Cmn Form Pharmacy
 Drug Channels Catching Up With Valeant And Walgreens And Their New Best Friend
Drug Channels Catching Up With Valeant And Walgreens And Their New Best Friend
 Drug Channels Taking Specialty Prior Authorization From 5 Days To 5 Minutes
Drug Channels Taking Specialty Prior Authorization From 5 Days To 5 Minutes
 Brilliant Medicare Part D Prior Authorization Form For Medication Models Form Ideas
Brilliant Medicare Part D Prior Authorization Form For Medication Models Form Ideas
Https Www Explainmybenefits Com Wp Content Uploads 2019 02 Rx Priorauthorization Pdf
 Specialty Pharmacy Fill Online Printable Fillable Blank Pdffiller
Specialty Pharmacy Fill Online Printable Fillable Blank Pdffiller
 Walgreens Application Pdf Fill Out And Sign Printable Pdf Template Signnow
Walgreens Application Pdf Fill Out And Sign Printable Pdf Template Signnow

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.