Fax your written appeal to 1-888-458-1406. Care Health Plan to provide Medi-Cal Managed Care services in Los Angeles County.
Https Www Anthem Com Ca Provider F3 S1 T4 Pw E224354 Pdf Refer Agent
ANTHEM is a registered trademark of Anthem Insurance Companies Inc.
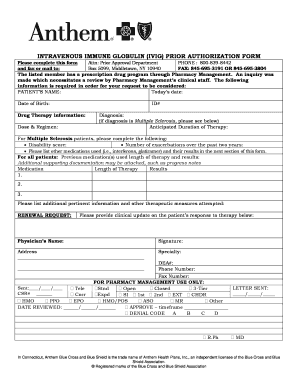
Anthem blue cross medi cal prior authorization form. For telephone prior authorization requests or questions please call 1-855-817-5786. Medical Pre-Authorization Request Anthem Blue Cross is the trade name of Blue Cross of California. AWIPEC-0649-18 January 2018 Prior Authorization Form for Medical Injectables If the following information is not complete correct andor legible the prior authorization PA process can be delayed.
The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan. For a full list of forms visit Anthems website. We are currently in the process of enhancing this forms library.
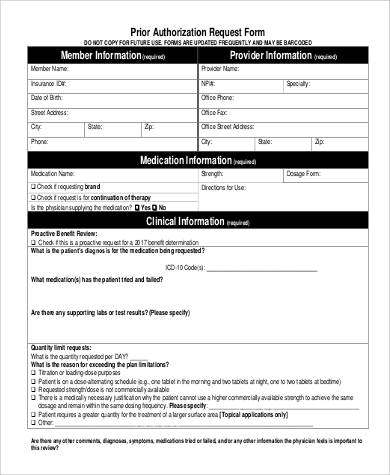
This form is only to be used if you are on the Anthem HMO or HSA plans. The Blue Cross and Blue. Utilization Management Case Intake Forms.
Care Health Plan to provide Medi-Cal Managed Care services in Los Angeles County. The Blue Cross name and symbol are registered marks of the Blue Cross Association. Pharmacy Claim Form Note.
Blue Cross and Blue Shield Association. An incomplete incorrect or illegible form will delay the prior authorization PA process. Medication information Drug name and strength requested.
Electronic Data Interchange EDI Prior Authorization. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. For Synagis or other medical injectable drug prior authorizations please call 1-866-323-4126.
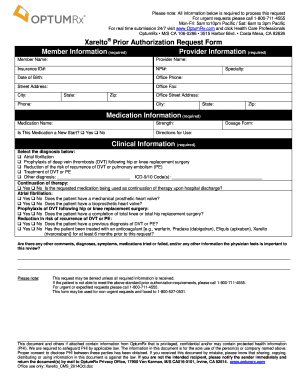
Blue Cross of California is contracted with LA. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost. Anthem Medical Specialty Pharmacy Anthem Med SRx Prior Authorization Drug List Prior authorization is the process of reviewing a drug treatment or other service in advance to determine if it meets the plans clinical criteria or if it is not medically necessary andor investigational under the criteria.
SIG dose frequency and duration. Please complete one form per member. ANTHEM is a registered trademark of Anthem Insurance Companies Inc.
To verify pharmacy network participation or Anthem Blue Cross Anthem. Blue Cross of California is contracted with LA. Pharmacy Prior Authorization Center for Anthem Blue Cross Cal MediConnect Plan Medicare-Medicaid Plan.
List all current medications including dose and frequency. Anthem Blue Cross and Anthem Blue Cross Life and Health Insurance Company are independent licensees of the Blue Cross Association. 711 Monday through Friday from 8 am.
ACAPEC-0019-13 122013 947730 122013 Community-Based Adult Services CBAS Authorization for Treatment Policy for New Anthem Blue Cross Members This provider bulletin is an update about the process for obtaining treatment authorization. Provider Forms Guides Easily find and download forms guides and other related documentation that you need to do business with Anthem all in one convenient location. Policies Guidelines.
Our Interactive Care Reviewer ICR tool via Availity is the preferred method for submitting prior authorization requests offering a streamlined and efficient experience for providers requesting inpatient and outpatient medical or behavioral health services for our. The Blue Cross name and symbol are registered marks of the Blue Cross. Enhanced Personal Health Care.
For telephone PA requests or questions please call 1-866-363-4126. Please allow Anthem Blue Cross at least 24 hours to review this request. Please fill out the Prescription Drug Prior Authorization Or Step Therapy Exception Request Form and fax it to 877 327-8009.
Select the Drug List Search tab to access up-to-date coverage information in your drug list including details about brands and generics dosagestrength options and information about prior authorization of your drug. Call Member Services at 1-855-817-5785 TTY. Anthem has also made available a series of forms for specific medications.
Anthem Blue Cross Cal MediConnect Plan MMP Complaints Appeals and Grievances 4361 Irwin Simpson Road Mailstop OH0205-A537 Mason OH 45040. After you have completed this form fax it to 1-888-708-2584. This call is free.
ANTHEM is a registered trademark of Anthem Insurance Companies Inc. You can get additional help about a Medi-Cal service. Anthem Blue Cross Anthem is available by fax or Interactive Care Reviewer ICR 247 to accept prior authorization requests.
Patient Care Patient Care. Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. Use one form per member.
Please allow Anthem at least 24 hours to review this request. Services Requiring Prior Authorization The table below outlines the services that require Prior Authorization PA for Anthem Blue Cross Medicaid Business members enrolled in Medi-Cal Managed Care Healthy Families Program HMO and EPO Access for Infants and Mothers AIM Program HMO and EPO and Major Risk Medical Insurance Program MRMIP. Anthem Blue Cross Pharmacy Prior Authorization Form Page 2 of 2 Describe medical necessity for nonpreferred medications or for prescribing outside of FDA labeling.
Fax this form to 1-844 -494 8341. Diagnostic studies andor laboratory tests performed.