All Marketplace plans must cover treatment for pre-existing medical conditions. 1 If you were applying for insurance in the individual market some health insurance companies would accept you conditionally by providing a pre-existing condition exclusion period or a full exclusion on the pre-existing condition.
 Pre Existing Conditions And Medical Underwriting In The Individual Insurance Market Prior To The Aca Kff
Pre Existing Conditions And Medical Underwriting In The Individual Insurance Market Prior To The Aca Kff
A pre-existing condition is defined as any ailment illness or condition where in the opinion of a medical adviser appointed by the health insurer the signs or symptoms of that illness ailment or condition existed at any.

Switching health insurance with pre existing condition. Question about switching health insurance plans and switching to a health insurance different provider Health Insurance 4 replies All times are GMT -6. All pre-existing conditions are covered under the Affordable Care Act Obamacare Insurers cannot deny health coverage for people for pre-existing conditions. It is important to understand how your pre-existing condition impacts your health insurance application and whether you would be able to make a claim for your pre-existing condition in the future.
However there may be health plans that are a better fit for you than others if you have a chronic or pre-existing medical condition. Pre-existing Condition and NY. In order to do this we first need to explain how a health insurance provider will consider your application a process known as underwriting.
No insurance plan can reject you charge you more or refuse to pay for essential health benefits for any condition you had before your coverage started. Insurers cannot charge higher costs or subject people with pre-existing conditions. Defining pre-existing health care conditions changes from state to state because it was never nationalized but the exclusion of certain pre-existing health care conditions is standard in all states.
Most short-term plans also do not cover treatment of pre-existing medical conditions If you go with this option then you must be certain that your pre-existing conditions will be covered and that the coverage will transfer to the new employee health plan without a hitch via HIPAA when you become employed again. A pre-existing condition is a health problem you had before the date that your new health coverage starts. So if you have a pre-existing condition you would likely lose your insurance and be left uninsurable.
For existing customers if you switch over to a different insurer it may be that you will lose the additional benefit accrued with us for your pre-existing conditions as many. A pre-existing condition is defined as a health condition that a person has before applying for a health insurance policy or getting a new health plan. A health insurer cannot deny you coverage or raise rates for plans if you have a medical condition at the time of enrollment.
Pre-existing conditions include epilepsy cancer diabetes lupus sleep apnea and many more. Law 4318 a and b McKinney 2000 Question Presented. One that was treated in the last 6 months your new group health plan can only exclude the condition from your coverage for a maximum of 12 months.
Once youre enrolled the plan cant deny you coverage or raise your rates based only on your health. Can a health insurance company deny me or charge me more for my pre-existing condition. Existing customers and your pre-existing conditions rolling benefit.
A pre-existing condition is any health condition or injury you have before enrolling in a health insurance plan. But you can still buy the policy by adhering to certain terms and conditions put by the health insurance companies. Therefore they do what they can to minimize losses.
If you do have a pre-existing medical condition ie. Did a Health Maintenance Organization err by denying coverage for a pre-existing health condition. Choosing a health plan is no longer based on the concept of a pre-existing condition.
It can be used to determine the premium you pay for your health coverage. Health insurance companies are generally reluctant to cover individuals with pre-existing illness due to higher chances of recurrent claims in the future. An insurance company cant deny you charge you more or.
Pre-Existing Conditions Under current law health insurance companies cant refuse to cover you or charge you more just because you have a pre-existing condition that is a health problem you had before the date that new health coverage starts. The Office of General Counsel issued the following informal opinion May 21 2001 representing the position of the New York State Insurance Department. Moreover the new insurance company must give you credit for continuous health coverage that you had prior to enrolling in the new plan.
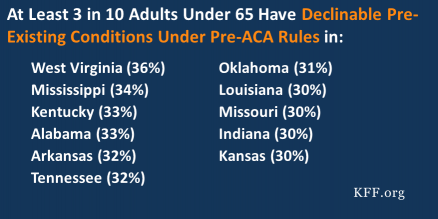
Health insurers are in business to make profit. Pre-ACA a pre-existing condition could affect your health insurance coverage. These rules went into effect for plan years beginning on or after January 1 2014.
Terms and Conditions for Health Insurance with Pre-existing Diseases. This is where the waiting period comes into play for individuals who have gone without any medical health insurance coverage for over six months. Under the Private Health Insurance Act 2007 a health insurer may impose a 12 month waiting period on benefits for hospital treatment for pre-existing conditions.
