Chemical peels are almost always considered a cosmetic procedure and insurance rarely covers it. But they also have higher risks and have a longer healing time than light or medium peels.
 Chemical Peel Free Consultation Your Skin Our Care Huidtherapeut Nl
Chemical Peel Free Consultation Your Skin Our Care Huidtherapeut Nl
Experience Weve been working with businesses like yours for over 35 years.

Chemical peel insurance. This type of treatment uses a chemical solution that is applied to the skin which causes it to blister up. Youll be paying for the procedure out of pocket. Depending on your specific needs and your dermatologists recommendation you may choose a chemical peel option that ranges from very light just the surface of the skin to improve uneven skin tone and other mild symptoms or you may choose a chemical peel that goes deeper to address fine lines wrinkles scars including acne scars adult acne symptoms and other concerns.
This process destroys the top layers of the skin in a controlled way so that new skin can grow in its place. They help remove dead skin and also begin to stimulate the growth of new skin. The longer answer requires you to read some definitions from the American Medical Association AMA.
As it is a procedure that actually damages the skin in a controlled manner complications can arise and chemical peels run the risk of causing irreversible damage to the skin in the form of scarring. The main three types of peel you will come across are superficial medium and deep. What Is Chemical Peel Treatment Insurance.
There are different types of chemical peels. Chemical peels are widely used by many to rejuvenate and bring life to our skin. Laser skin whitening before after breast cost reduction tn knoxville At Solihull Dental Centre Implant Clinic in Solihull we provide our patients with Cosmetic Dentistry In a relaxed and friendly atmosphere to be a member of the British Dental.
What are chemical peels. Results are immediate and can be very effective. So does insurance pay for a chemical peel.
With insurance coverage out-of-pocket costs for a chemical peel. J Cutan Aesthet Surg. Your initial consultation visit however may be covered by insurance.
Chemical peels are considered cosmetic procedures and are not covered by health insurance. Chemical Peel Covered By Insurance Are Different Thigh Lifts Types What. Chemical peels are used to improve the appearance of the skin.
Read more on Beauty and Bodywork Insurances blog. Youll be paying for the procedure out of pocket. Your initial consultation visit however may.
Handog EB Datuin MS Singzon IA. Does insurance cover chemical peels. Does insurance cover the cost of a chemical peel.
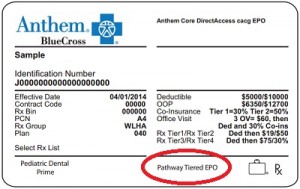
Deeper peels give more noticeable results. Most health insurance plans dont cover the cost of chemical peels unless the health insurer considers the treatments to be medically necessary. If you cant afford the procedure up front many doctors offices have financial plans.
However this will usually be rare since most insurance companies only see it for aesthetic purposes. I had a lower body lift but I didnt need much muscle repair so I think my procedure was lessI ended up having to get a revision done for dog ears on the side so it. Chemical Peel Insurance Coverge List Procedures Cosmetic Price Pasadena Cosmetic Surgery is a specialty practice dedicated to delivering highly Dr.
Chemical peels are great for reducing acne and come in several forms. A chemical peel is a treatment to improve the look of the skin. However if a peel is being performed in order to remove a precancerous growth there is a possibility of it being covered.
Additionally does Medicare pay for skin cancer removal. Financial Strength Insurance provided by a Standard Poors A Stable rated insurer. If the procedure is needed to improve the appearance of a scar a chemical peel can be covered by insurance.
Just so is chemical peels covered by insurance. Chemical peels are almost always considered a cosmetic procedure and insurance rarely covers it. Chemical peels for acne and acne scars in Asians.
Chemical Peels are a popular treatment used to regenerate the skin without the use of invasive surgery. Chemical peels can be done on the face neck or hands. Passion Tailor-made insurance policies made for specialists by specialists.
Eventually this blistering peels off to reveal smoother and less wrinkled skin than the old skin. What is Chemical Acid Peel Insurance. A professional who uses the chemical peel technique needs to have the financial protection that comes from having liability insurance in case something goes wrong with the procedure.
Chemical peel--current possibilities and limits.





:max_bytes(150000):strip_icc()/how-is-the-flu-diagnosed-770483_V3-33faae86c97749298f425df7e792f07a.png)

