You may also call LA. This number has 49 user reports.
Https Www Dhcs Ca Gov Services Ccs Documents Wcm 90 Day March2018 Pdf
All reports are written by real visitors of this website.
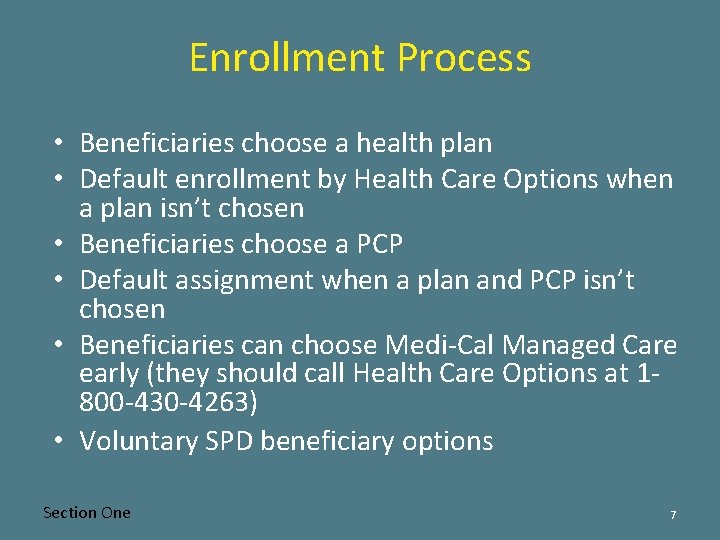
800 430 4263. Other ways of searching this number are. For TDDTTY users call 1-800-430-7077. Assistance filling one out call 1-800-430-4263.
Monday through Friday or visit their website. Contact Medi-Cal Managed Care Call. 800 269 0271 Reply.
You can call between 800 am. 1 800-430-4263 International format sometimes is written as 1-800-430-4263 or just 18004304263 800 430-4263 Domestic format sometimes is written as 800-430-4263 or just 8004304263. To switch your Medi-Cal plan you can call Medi-Cal Managed Care Health Care Options at 1-800-430-4263.
Report unwanted calls to help identify who is calling. Call them back and answer their questions so you covered. 8004304263 1-800-430-4263.
1 comments were added to this telephone number. Call Health Care Options at 1-800-430-4263 to request your Medi-cal Choice Enrollment Form. Call Health Care Options at 1-800-430-4263 TTY.
You can also send in the postcard that you received from Health Care Options to get your Medi-cal Choice form. The company that called you. You filled out a form to receive healthcare.
1 800 430-4263 Call type. Anthem Blue Cross Partnership Plan Standard Benefits Doctor Visits Specialist Services Pharmacy Hospital Care inpatient and outpatient Emergency Services 24 hours a day 7 days a week Prenatal Care Newborn and Well-Baby Care Family Planning Services Vision. That number is 800 430-4263.
Covid Information Reply. Ashton Posted 26 Mar. Riley Posted 09 Jul 2019.
Care Member Services at 1-888-839-9909. Complaint Statistics Consumers from California Minnesota New York Utah complained about phone number 8004304263 calls or text messages. Reverse phone lookup for 800 430-4263.
This phone number is trying to call me many times a day and asks for my SSN. Questionable calls elusive and claim to be government. Questionable calls elusive and claim to.
Phone 8004304263 has a negative user rating. View Owners Address. Call type Phone number or keyword you want to search for.
If you want to try another plan available in your county you can change it at any time. 8 May 2014 1 reply. 1-844-580-7272 TTY 1-800-430-7077 We are open Monday through Friday 8 am.
Report to Attorney Get at. Hello This is second time that a strange number is calling me and dont speaking. When i pick up NO response.
Report a phone call from 800-430-4263. Please contact California health care options at 1-800-430-4263 at your earliest convenience. 1-800-430-4263 TTY 1-800-430-7077 Coordinated Care Initiative.
Find the 800 430-4263 callers full name address email and photos at Spokeo. So far 1 users have classified this telephone number as Unknown. Please check information users rating and reports about phone number 800-430-4263.
Phil replies to Amir. Directory of UNKNOWN Callers. You filled out a form to receive healthcare insurance and gave your number.
800-430-4263 summary and related numbers. Read comments below to find details about this number. Someone named Clovis asking about healthcare and my SS I didnt give it to them.
This phone number is registered in Toll Free and operated by. You may also complete a Medi-Cal Choice Form that you can find on the Health Care Options download page. 1-800-430-7077 to choose a new plan.
The number may be unsafe. Cass Posted 26 Feb 2021. Get a call from 8004304263.
Number 8004304263 reportsSCAMSPAM SUSPECTED. Searches User Comments Leave a Comment July 10th 2019 1227am. 1 800-430-4263 8004304263 800-430-4263.
The last time it was checked was 04302021. The telephone number 800-430-4263 was being searched 45 times. Look for the Medi-cal Choice enrollment form in the booklet.
This number 800 430 4263 calls me twice or more a day. I wasnt covered and ran up a 20K medical bill because I didnt. Is this number a spammer.
This brochure details how to complete your application. 1-800-430-4263 Receive a welcome packet from your plan Enjoy your new benefits.





