If you are looking for dental and vision coverage we can help. I want you to be wary as certain Medicare plans especially around Medicare Advantage can include extra dental or vision benefits.
 Does Medicare Cover Dental Healthline Com
Does Medicare Cover Dental Healthline Com
Premium for the Dental Vision Hearing Package may be re-evaluated each year and is subject to change.
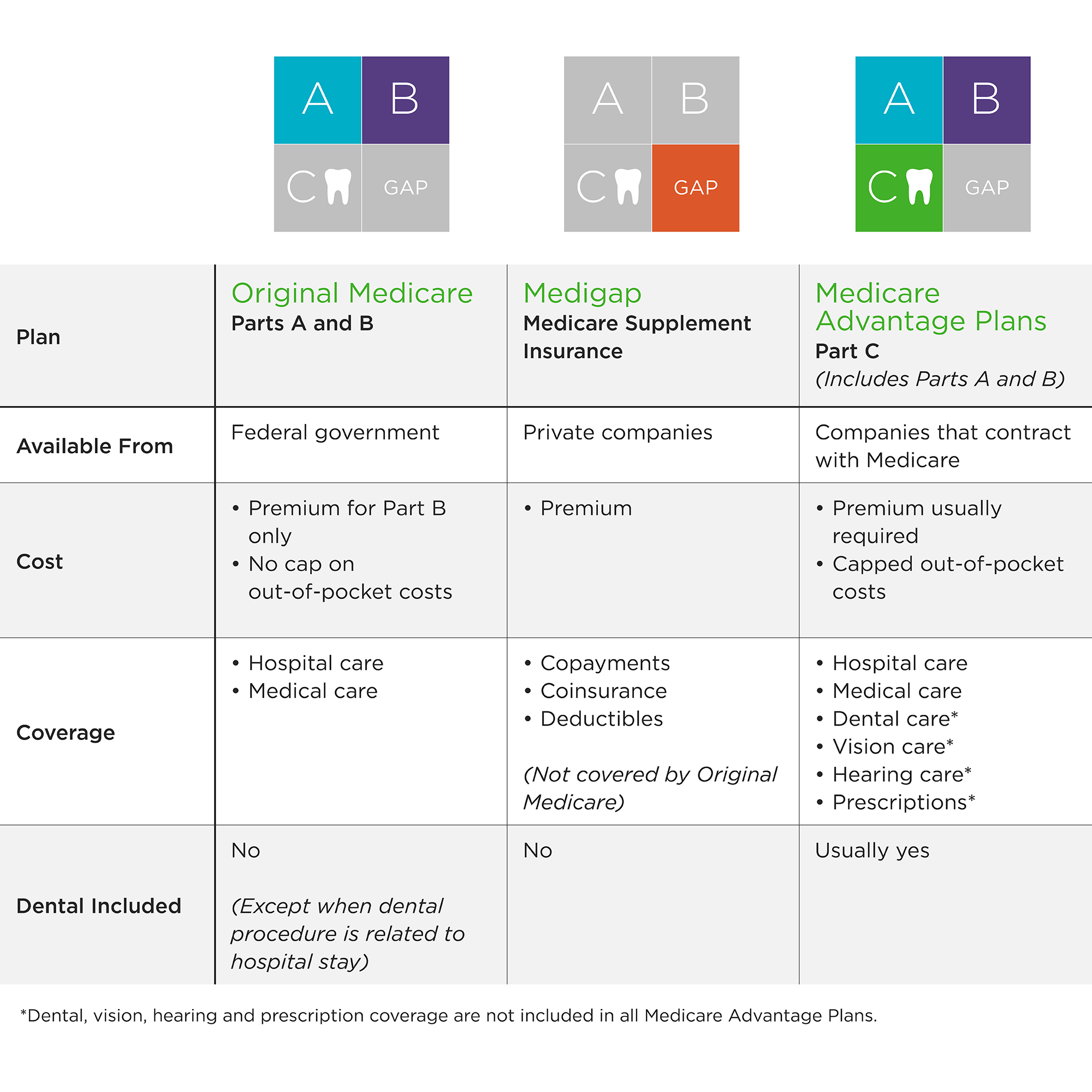
Do medicare supplement plans cover dental or vision. If you want dental coverage consider Medicare Advantage plans. It is important that you contact your provider before you settle on a plan. Most also include prescription drug coverage as well as other benefits such as hearing health coverage and gym memberships.
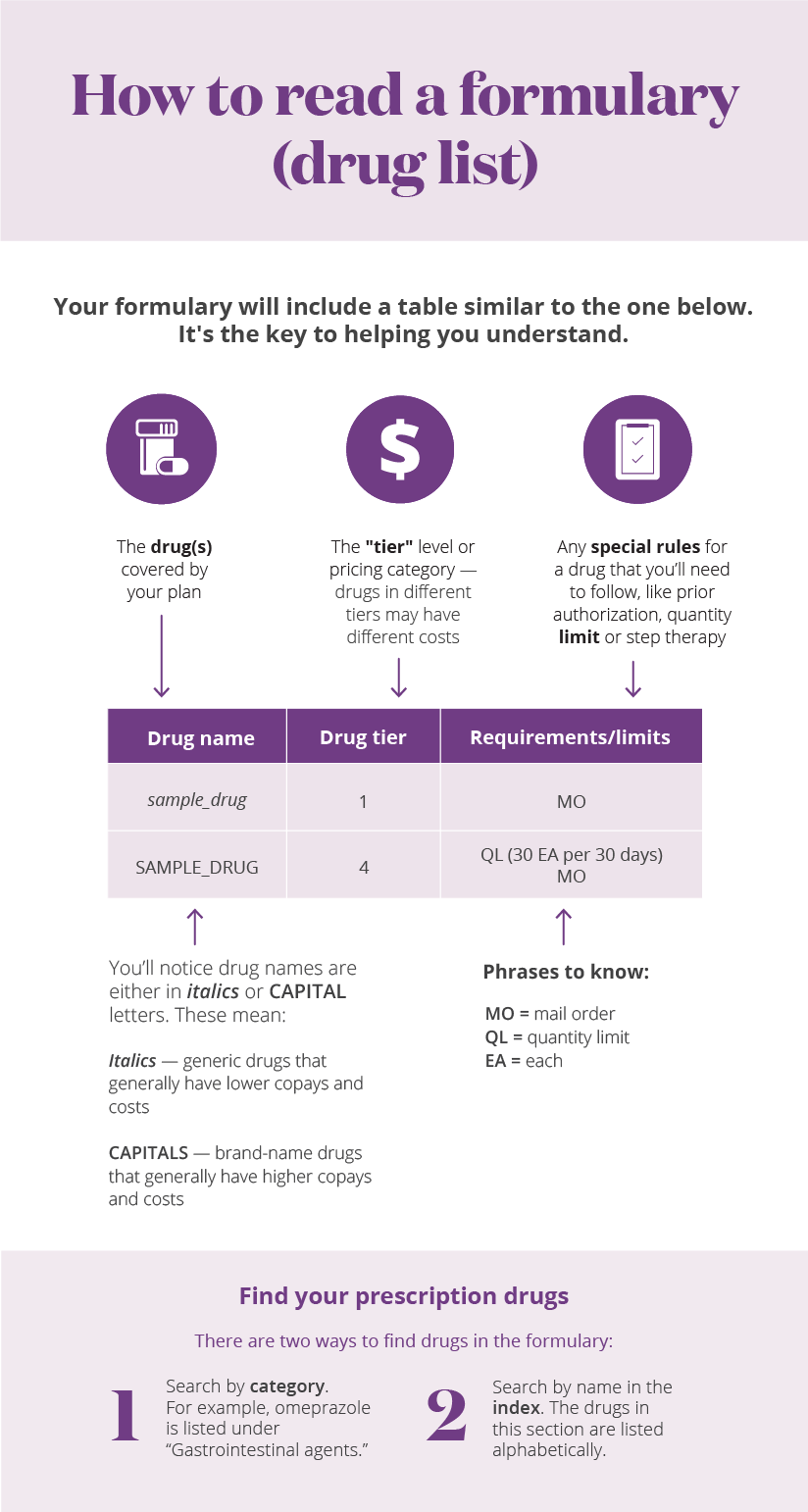
Dental PPO 1500 plan for all Medicare Supplement dental plan members have a 12-month waiting period and Dental PPO 1000 dental plan members have a 6-month waiting period for major restorative services and procedures such as crowns endodontics periodontics oral surgery and removable or fixed prosthetics. Your Medicare supplement plan provides even more value when you add the Dental Vision Hearing Package to your plan. A Medicare Supplement Insurance Medigap policy can help pay some of the remaining health care costs that Original Medicare does not cover.
Neither Medicare nor Medigap cover routine dental care such as teeth cleaning fillings and tooth extractions. Medigap can cover your Part A deductible and coinsurance. Original Medicare doesnt cover most dental care.
Instead these plans provide coverage for some of the out-of-pocket costs associated with Original Medicare such as deductibles copayments and coinsurance. How to Get SeniorDental and Vision. With your Medicare Supplement plan enrollment.
Many plans also include other coverage such as dental vision and hearing According to the Kaiser Family Foundation KFF a non-profit organization focusing on. Medicare Supplement Insurance plans do not cover dental services. If you are applying to become a Medicare Supplement plan member you can sign up for a Blue Shield dental plan at the same time by selecting a plan on the Medicare Supplement plan application.
However there is coverage for emergency oral surgery that takes place in the hospital. While Medicare Supplement Insurance Medigap and Original Medicare Medicare Part A and Part B do not cover routine dental and vision care Medigap plans can help beneficiaries pay for costs they may face if they get dental or vision care that are covered by Medicare. Medicare Supplement and Medicare Advantage are not the same thing.
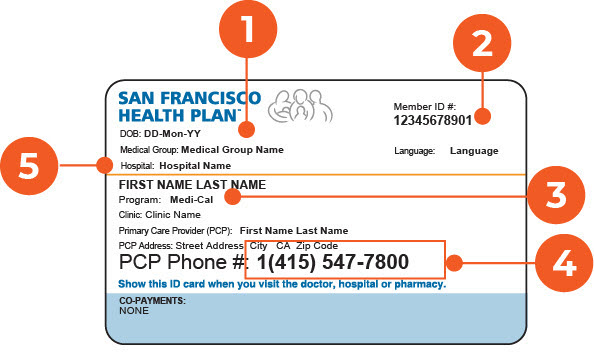
A supplement plan may not cover long-term care vision or dental care hearing aids eyeglasses or. Dental and vision benefits are built right into some of our Medicare plans. You and your other household member need to select and enroll in the same dental plan Become a member today.
If youre shopping for coverage for routine dental care such as teeth cleaning and X-rays and other dental care for fillings extractions dentures and more then Original Medicare doesnt cover those things. This may include copayments coinsurance and deductibles. Because Original Medicare Part A and Part B provide coverage for care that is medically necessary they do not help pay for routine vision and dental care such as regular examinations teeth cleanings or fillings tooth extraction eyeglasses or contact lenses.
Not everything falls under Medigap however. In some states we also have dental and vision packages that you can add on to another plan or purchase separately. This includes cleanings fillings extractions dentures dental plates and other devices.
However if you suffer a dental emergency and must visit the hospital a Medicare Supplement Insurance plan may cover your Medicare Part A deductible and copayment as well as your Medicare Part B deductible. In my opinion the big hole is around dental. Blue Cross Medicare Supplement plans do not include routine dental exams cleanings and X-rays.
But not all vision and dental care is. Medicare Supplement Insurance also called Medigap does not provide coverage for dental or vision care. Medicare Advantage plans are offered by private insurance companies.
Picking the right Medicare insurance is essential to make sure you have the coverage you need moving forward. Typically that can be enough vision coverage for most people. There are also other types of Medicare plans called Medicare Advantage plans that may provide routine dental and vision.
Medicare Advantage MA plans provide Part A hospital coverage and Part B medical coverage plus additional coverage like prescription drugs vision hearing and dental health. Medicare Advantage Part C plans can offer coverage for dental and vision health items in addition to also offering the same coverage as Original Medicare. Learn more about our vision coverage to help you to support your eye care needs.
You may choose to pair a new or existing Blue Cross Medicare Supplement or Legacy Medigap plan with the Dental Vision Hearing Package that includes coverage for fillings root canals extractions crowns and fluoride treatments. For 1525 a month you can add dental vision and hearing coverage to enhance your Medicare supplement plan. I DO NOT recommend that you make a Medicare decision based simply on dental or vision coverage.
Most Medicare Advantage dental plans cover dentures and much more cleanings x-rays annual exams fillings pullings and root canals. Original Medicare does not cover most dental services. Part C offers additional benefits that Original Medicare wont cover like dental vision or hearing.
Learn more about our dental coverage to supplement Medicare.