A non-preferred drug is a drug that is not listed on the Preferred Drug List PDL of a given insurance provider or State. 6 pm Eastern time Please note.
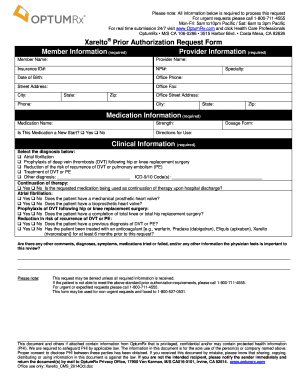 Optumrx Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
Optumrx Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
Prescribers can submit their requests to Humana Clinical Pharmacy Review HCPR in the following ways.
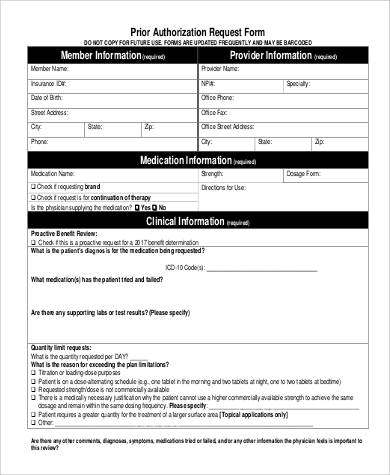
Prior authorization request. A provider or supplier submits either the prior authorization request or pre-claim review request. A prior authorization PA sometimes referred to as a pre-authorization is a requirement from your health insurance company that your doctor obtain approval from your plan before it will cover the costs of a specific medicine medical device or procedure. Prescription prior authorization forms are used by physicians who wish to request insurance coverage for non-preferred prescriptions.
Requesting Prior Authorization If youre enrolled in a TRICARE Prime plan your primary care manager PCM will work with your regional contractor for the prior authorization. Prior authorization is required for some membersservicesdrugs before services are rendered to confirm medical necessity as defined by the members health benefit plan. However the provider or supplier can render services before submitting the request.
Prior authorization PA is often used with expensive prescription drugs. Under pre-claim review the provider or supplier submits the pre-claim review request and receives the decision prior to claim submission. Health insurance companies use prior authorization to verify that a certain drug procedure or treatment is medically necessary before it is done or prescribed.
Prior Authorization Requests PARs. How to request prior authorization. What is a Prior Authorization.
Prior authorizationsometimes called precertification or prior approvalis a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage. Within a week you can call your pharmacy to see if the prior authorization request was approved. The AMA believes that the overall volume of medical.
Drug-Specific Prior Authorization Forms 2021 Use the appropriate request form to help ensure that all necessary information is provided for the requested drug. Under prior authorization the provider or supplier submits the prior authorization request and receives the decision prior to rendering services. Your doctor may also recommend an alternative medication for youone that is equally effective and covered by your plan.
Typically within 5-10 business days of hearing from your doctor your health insurance company will either approve or deny the prior authorization request. All supporting medical documentation andor any additional pertinent information should be included when submitting this form. You need to contact your regional contractor for prior authorization.
If it wasnt you can call your insurance company to see why the authorization was delayed or denied. Providers request authorization for services before providing certain services. Prior authorization sometimes called preauthorization or pre-certification is a pre-service utilization management review.
The notification will include applicable timeframes for the provider to submit the requested information. Without this prior approval your health insurance provider may not pay for your medication or operation leaving you with the bill instead. Non-Formulary Drug Prior Authorization Form Use this request form if the medication you want to request does not.
For all other plans. Prior authorization is a requirement that your physician obtains approval from your healthcare provider before prescribing a specific medication for you or to performing a particular operation. Submitting a request for prior authorization A request must be submitted and approved in advance for medications requiring a prior authorization before the drugs may be covered by Humana.
Submit a Request for Prior Authorization and Notification Check the Status or Update a Previously Submitted Request for Prior Authorization Upload Medical Notes or Other Attachments to a Request Information on Prior Authorization Programs for Cardiology Oncology Radiology Clinical Pharmacy and Specialty Drugs. Online preauthorization requests are encouraged. The ColoradoPAR vendor reviews the request to determine if services are medically necessary according to established criteria and guidelines.
If a prior authorization request lacks the necessary information to determine medical necessity we will send a letter describing the documentation that needs to be submitted to the member and the requesting provider within 3 business days from receipt of the request. Except where noted prior authorization requests for medical services may be initiated. If its rejected you or your doctor can ask for a review of the decision.
Prior authorization can take days to process.










