If you use out-of network providers without a referral or authorization payment will not be made by Tufts Health Plan Medicare Preferred. 24-34-114 Out-of-network health care providers Out-of-network services Billing Payment.
See Chapter 6 Section 100 Special Rules for Services Furnished by Non-Contract Providers.

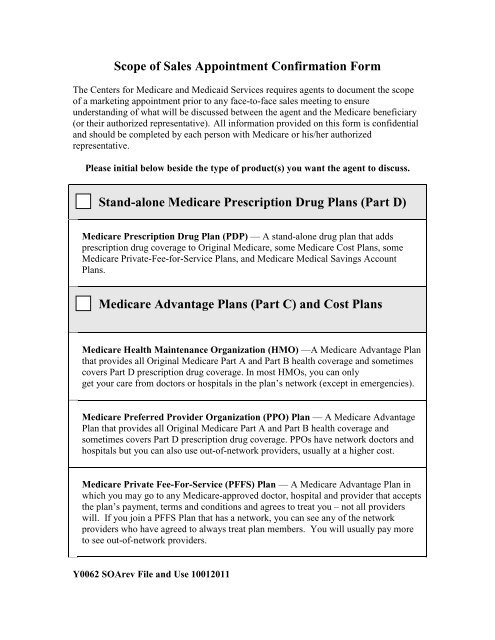
Medicare out of network provider. Here are other important things to know about using out-of-network providers. These circumstances include seeing a provider with a specialty not currently contracted with our plan. At the most basic level when a Medicare Advantage HMO member willingly seeks care from an out-of-network provider the member assumes full liability for payment.
Colorado Revised Statute. This is a doctor hospital or other provider not on your health plans list of network providers. You will receive the majority of your healthcare services from your PCP.
Medicare Advantage Plan Part C offered by a private insurance company. 110 percent of the carriers median in-network. Out-of-network emergency and non-emergency services are reimbursed at the greater of.
If out-of-network providers accept more than Original Medicare amounts for services rendered they are subject to penalties. Because the vertigo struck while on vacation Mary had little choice but to go to an out-of-network provider. Each plan has in-network and out-of-network providers.
If your provider misses the filing deadline they cannot bill Medicare for the care they provided to you. A Special Needs plan SNP is like an HMO in the way that you can only go out of network for emergency and urgent care or if you traveling and. Some insurance plans use Medicare fees as a basis for reimbursing service for out-of-network providers.
Your Primary Care PhysicianProvider PCP must be part of our network. Established a payment methodology maximum for out-of-network services. If you receive a bill from a provider who is not part of Prominence Health Plans network please do not pay the bill.
Providers who take assignment should submit a bill to a Medicare Administrative Contractor MAC within one calendar year of the date you received care. Opt-out providers do not bill Medicare for services you receive. This document is a general outline of Medicare payments as of the above date and as such does not contain many of the payment details.
Can I Bill as an Out Of Network Provider for Medicare Part B. Medicare Supplement Medigap plans also generally dont have networks. They then multiply that fee by a certain percentage to set the maximum amount that they will pay for that procedure.
You can get your care from an out-of-network provider however in most cases that provider must be eligible to participate in Medicare. That is neither the HMO plan nor TM will pay for services when an MA member goes out-of-network. The long answer is that its a huge pain in the butt.
So the long and the short of it is that if you dont have a physical Medicare contract and you havent. PPO Plans have network doctors other health care providers and hospitals. Depending on the circumstances if you see an out-of-network provider you may have to file a claim to be reimbursed by the plan.
If you go out of network your insurer may pay for part of the bill. Under limited circumstances our plan will allow our members to see out-of-network providers. But there may be times when you receive care from an out-of-network provider.
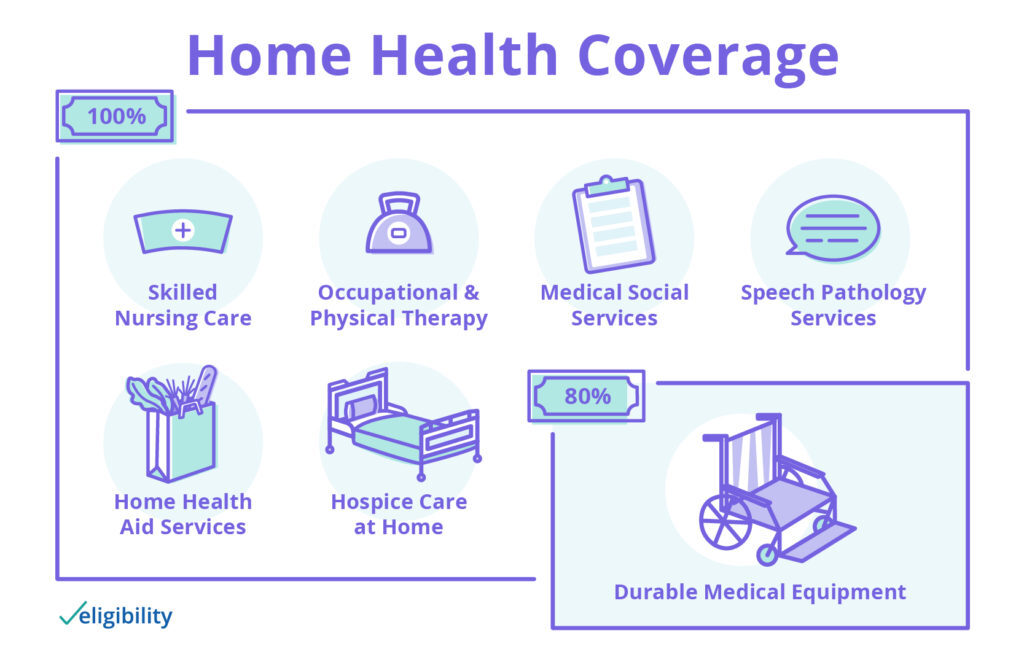
Your insurance company then pays the rest of the bill. If you have Original Medicare Part A and Part B you typically can receive care from any Medicare provider that accepts assignment Assignment means that the provider accepts the Medicare-approved amount as full payment for covered services. Except for emergency care we cannot pay a provider who is not eligible to participate in Medicare.
For basic care like check-ups youll probably pay the same amount for any in-network provider you see. You may be able to go out of network for certain services for example if you need to see a specialist and the plan doesnt cover the type you need to see in your area. Required to pay at least the original Medicare rate to out of network providers.
Generally if you have an HMO plan you pay less if you get care from a network Medicare doctor. The short answer is definitely not. Your copayment or coinsurance.
Visiting an out-of-network provider often results in higher costs to the beneficiary. You pay more if you use doctors hospitals and providers outside of the network. When you use in-network providers you pay a certain set part of the bill.
You pay less if you use doctors hospitals and other health care providers that belong to the plans Network. Many psychiatrists opt out of Medicare. The basic Medicare Advantage out-of-network payment rule is that health care providers who treat Medicare Advantage enrollees on an out-of-network basis must accept as payment in full amounts the provider would have collected if the patient were enrolled in original Medicare.
Authorization is required on a case by case basis and the billing is a nightmare. The payment rates described in this document do not apply to a plans network providers. The rate is often less than what your doctor charges.
In practice some providers have signed contracts as in-network providers that reimburse SNFs and HHAs at less than FFS Medicare.


/UnitedHealthcare-dd464c44145549308e61d36a8869e9f8.png)