Not all services and drugs need preauthorization. Independent licensee of the Blue Cross and Blue Shield Association.
Https Www Empireblue Com Provider Noapplication F3 S2 T2 Pw Ad067834 Pdf Refer Ehpprovider
Program Phone number HIP 1-844-533-1995.
Anthem blue cross blue shield prior authorization fax number. Monday to Friday 7 am. Anthem Blue Cross and Blue Shield is a DSNP plan with a Medicare contract and a contract with the state Medicaid program. Rocky Mountain Hospital and Medical Service Inc.
Please fill out the Prescription Drug Prior Authorization Or Step Therapy Exception Request Form and fax it to 877 327-8009. We are currently in the process of enhancing this forms library. Select the Drug List Search tabto access up-to-date coverage information in your drug list including details about brands and generics dosagestrength options and information about prior authorization of your drug.
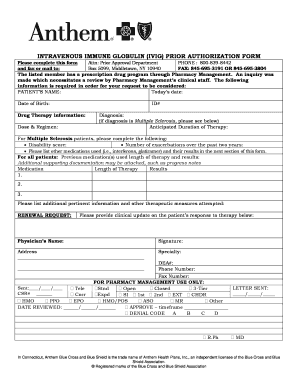
The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan. PrecertificationPrior authorization is the determinationby Anthem that selected. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification.
For both outpatient procedures and treatment requiring an inpatient stay call 800 633-4581 to obtain prior authorization. For prior authorization requests handled by AIM Specialty HealthSM AIM. Members of the Federal Employee Blue CrossBlue Shield Service Benefit Plan FEP are subject to different prior authorization requirements.
Participating and Nonparticipating Durable Medical Equipment Providers For durable medical equipment DME outpatient rehabilitation physical therapyoccupational therapyspeech therapy pain management home care home infusion or hyperbaric treatment and wound care please fax to 1-866-920-8362. Recommends submitting prior authorization requests for Anthem HealthKeepers Plus members via Interactive Care Reviewer ICR a secure Utilization Management tool available in Availity. Pharmacy Prior Authorization Center for Medi-Cal.
Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Maine Inc. By phone at 833-293-0659 or o. Easily find and download forms guides and other related documentation that you need to do business with Anthem all in one convenient location.
Submit your request to AIM in one of the following ways. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost. Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification.
The following guidelines apply to Anthem Blue Cross and Blue Shield Anthem products issued and delivered by Anthem in Connecticut. Online The AIM ProviderPortal is available 24x7. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required.
Log in to find contact information specific to your area and plan. Enrollment in Anthem Blue Cross and Blue Shield depends on contract renewal. To noon CT on weekends and holidays.
Weve provided the following resources to help you understand Empires prior authorization process and obtain authorization for your patients when its. During this time you can still find all forms and guides on our legacy site. Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of New.
Phone Call the AIM Contact Center at 800-859-5299 Monday through Friday 6 am. Health BH services using the following phone numbers. A preauthorization is the process where we review the requested service or drug to see if it is medically necessary and covered under the members health plan.
57 rows CO 23 Denial Code The impact of prior payers adjudication. For MediConnect Plan pharmacy requests please contact Anthem Blue Cross Cal MediConnect Plan Medicare-Medicaid Plan Customer Care at 1-855-817-5786. To 6 pm CT.
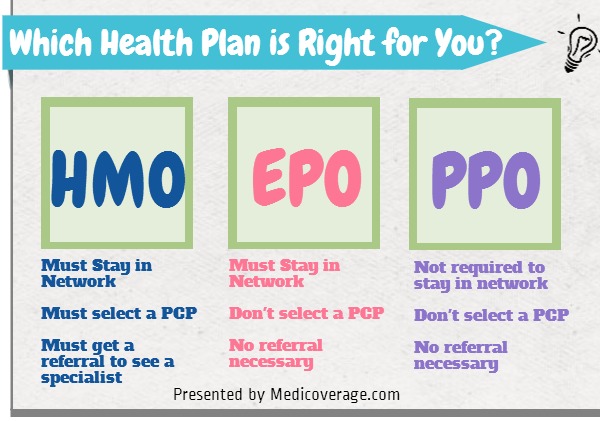
Anthem Blue Cross and Blue Shield Serving Hoosier Healthwise Healthy Indiana. Out -ofnetworkout area non emergency services HMOPOSBlue Direct HMO and Blue Open Access Only Mental health and substance abuse services including Residential Treatment -292 2879 or fax 866 737 8503. For information on precertificationprior.
Anthem Blue Cross and Blue Shield within 24 hours or the next business day. HMO products underwritten by. Preauthorization also called prior authorization or prior approval are a pre-service medical necessity review.
ICR offers a fast efficient way to securely submit prior authorization requests with clinical documentation. Contact Anthem Blue Cross and Blue Shield Customer Support in Indiana by phone or Live Chat. Anthem Blue Cross and Blue Shield is the trade name of.
Provider Forms Guides. Healthy Indiana Plan and Hoosier Care Connect How to obtain prior authorization cont Fax clinical information for all members to.