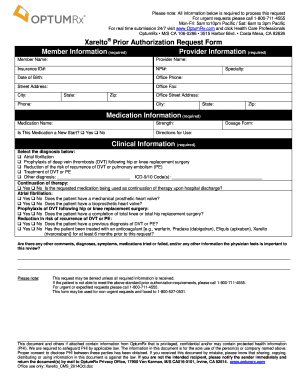
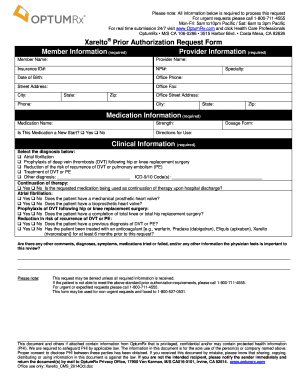
Prior Authorization Form for Medical Injectables If the following information is not complete correct andor legible the prior authorization PA process can be delayed. USFHP Pharmacy Prior Authorization Form.
 Optumrx Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
Optumrx Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
A standard form FIS 2288is being made availableby the Department of Insurance and Financial Services to simplify exchanges of information between prescribers and health insurers as part of the process of requesting prescription drug prior authorization.
Prior authorization form. Drug prior authorization - M6453 IHU PDF 129 kb. This form will be updated periodically and the form number and most. Service code if available HCPCSCPT.
A full list of CPT codes are available on the CignaforHCP portal. 888 819-1043 option 4. To do that well need information from you and your doctor about your plan your condition and what youre being prescribed.
There is no specific form to request prior authorization. Submit online at National Imaging Associates or call 1-800-642-7820. To ensure that prior authorizations are reviewed promptly submit request with current clinical notes and relevant lab work.
National Imaging Association NIA manages prior authorization for MRI PET CT scans nuclear cardiology and radiation oncology procedures. Start date of service. All requested data must be provided.
You can read more about the process in General information for prior authorization drugs PDF 12Mb. Use this form to request approval for a drug claim. 410 424-4607 or 410 424-4751.
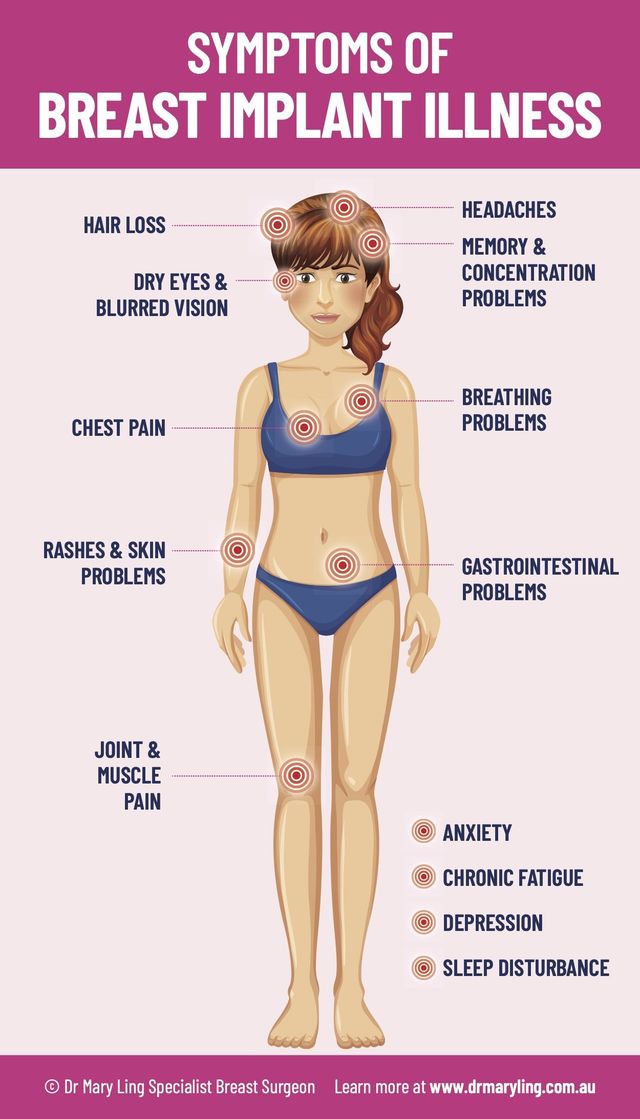
Prior Authorization Form Buprenorphine Products This document and others if attached contain information that is privileged confidential andor may contain protected health information PHI. Member Info Please Print Legibly NAME. Medical cannabis form - M6453 PDF 106 kb.
If you are accessing the Electronic Prior Authorization form via the Internet Explorer browser please click here for a guide to ensure all documents are transmitted. Incomplete forms or forms without the chart notes will be returned. Self Child Spouse.
FAX FAX Completed Form AND APPLICABLE PROGRESSCompleted Form AND APPLICABLE. Prior Authorization Information CVS Caremark Prior Authorization PA tools are developed to ensure safe effective and appropriate use of selected drugs. Some prescription drug claims need to be approved before you can apply for reimbursement.
FAX Completed Form AND APPLICABLE PROGRESS rNOTES to. Youll need the doctor to fill in some sections. Fax completed prior authorization request form to 877-309-8077 or submit Electronic Prior Authorization through CoverMyMeds or SureScripts.
Find a prior authorization form. The information in this document is for the sole use of OptumRx. Member information Last name First name Member ID number Date of birth - -.
Peer to Peer Scheduling Request Form - UnitedHealthcare offers the opportunity for your physician to speak with our medical director to discuss the medical policy and documentation requirements which determined the response for your prior authorization or concurrent review request. Contact the Pharmacy Dept at. Medicaid Rx Prior Authorization Forms The Medicaid prior authorization forms appeal to the specific State to see if a drug is approved under their coverage.
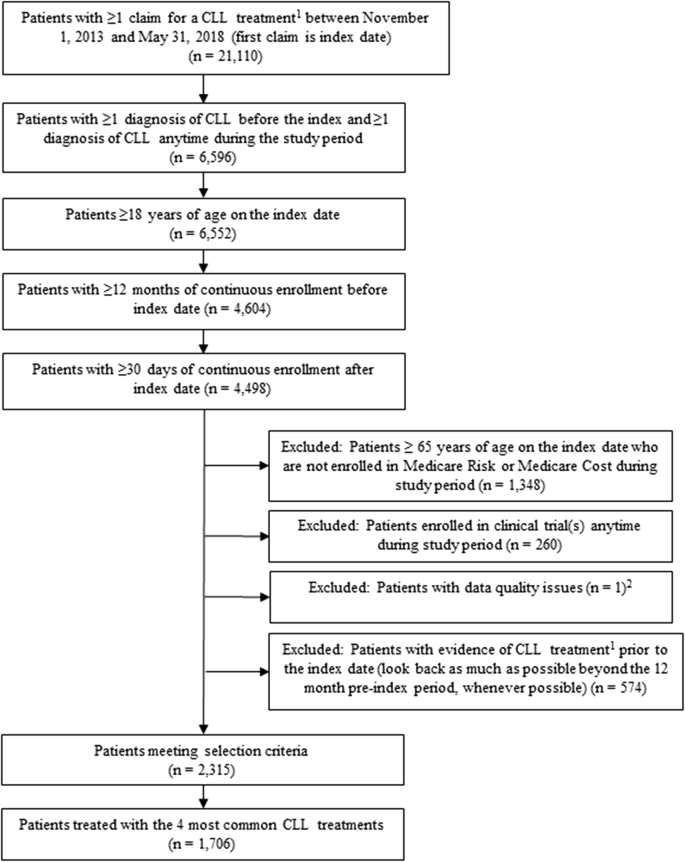
More forms can be found in the Clinical Pharmacy and Specialty Drugs Prior Authorization Programs section. If any items on the Medica Prior Authorization list are submitted for payment without obtaining a prior authorization the related claim or claims will be denied as provider liability. Prior Authorization Request Form Medica requires that providers obtain prior authorization before rendering services.
Provider - ePA saves administrative time by making it easier to submit and track prior authorizations and enables faster. Generate a prior authorization by sending an eRx 1. Prior Authorizations Forms.
Use one form per member. Use this form to request approval for medical cannabis coverage. Prior Authorization can ensure proper patient selection dosage drug administration and duration of selected drugs.
Prior authorization forms can be completed and submitted by any member of the practice from the patients Timeline the Prior authorization report or the Tasks section of the EHR. Your physician will need to fill out some sections. For Internal Use Only.
For Prior Authorization Requirements training tools submission options and user guides click here. 410 424-4607 or 410 424-4751. Completed Form AND APPLICABLE PROGRESS NOTES to.
Express Scripts manages prior authorizations and Non-Formulary requests for Medicare Part D prescriptions. Depending on a patients plan you may be required to request a prior authorization or precertification for any number of prescriptions or services. Choose a medication and fill in the order details.
PA Forms for Physicians. Pharmacy Prior Authorization Form. End date of service.
607 or 410 424-4751. Your Medicare Administrative Contractor MAC may make a cover sheet or other templates available. Medicare Part D Medications.
Member - ePA simplifies the prior authorization process ultimately getting members the medications they need faster minimizing disruption to therapy. The Provider named above is required to safeguard PHI by applicable law. Please include ALL pertinent clinical information with your Medical or Pharmacy Prior Authorization request submission.
This form is to be completed by the patients medical office to see if he or she qualifies under their specific diagnosis and why the drug should be used over another type of medication.