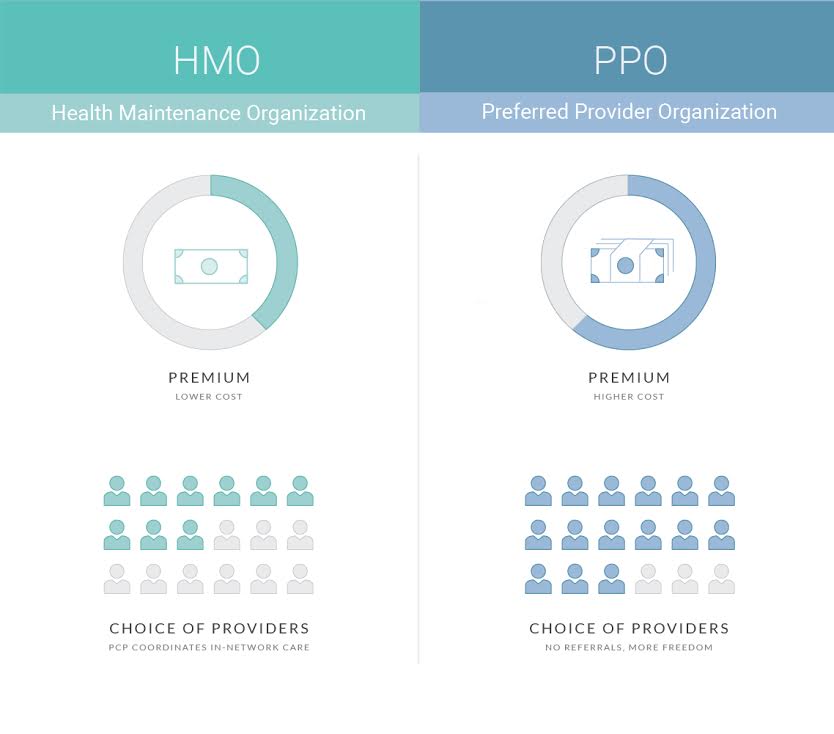
They also feature a network of providers but there are fewer restrictions on seeing non-network providers. The most significant difference between the two organizations is the option to select health care providers.
 Hmo Vs Ppo Vs Other Plans What S The Difference Insurance Com
Hmo Vs Ppo Vs Other Plans What S The Difference Insurance Com
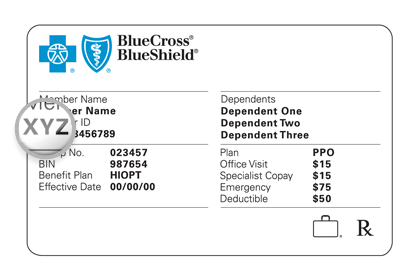
Sometimes referred to as a Participating Provider Organization or a Preferred Provider Option they are subscription-based medical care arrangements.
Whats a ppo. These providers have agreed to provide care to the plan members at a. With a PPO you have the flexibility to visit providers outside of your network. What Is a PPO.
Since HMOs only allow you to visit in-network providers its likely youll never have to file a claim. PPO stands for Preferred Provider Organization. A PPO allows you to choose from a larger pool of doctors than other plans requires a copay and typically has a higher monthly cost than other plansA PPO o.
Preferred Provider Organization PPO PPOs got that name because they have a network of providers they prefer that you use but theyll still pay for out-of-network care. This is because your insurance company pays the provider directly. That your order is effective immediately and can be enforced anywhere in Michigan That once it is served the PPO may be enforced anywhere else in the United States What actions the abuser is prohibited from doing When your order expires What happens if the abuser violates your.
A PPO is a kind of health insurance or managed care plan. A preferred provider organization PPO plan gives you access to a network of healthcare providers and medical facilities at reduced pricesgenerally. A PPO is a group of medical providers think doctors hospitals specialists therapists that partner with an insurance company.
PPO stands for Preferred Provider Organization. A PPO will state. These providers offer their services to the insurance plans members and subsequently the insurance company reimburses them predetermined rates.
PPO plans provide more flexibility when picking a doctor or hospital. To start HMO stands for Health Maintenance Organization and the coverage restricts patients to a particular group of physicians called a network. 2 HMOs and PPOs are both types of managed care which is a way for insurers to help control costs.
But in fact PPO out-of-pocket costs can climb quite high depending on the insurance company youre working with. A Preferred Provider Organization or PPO is a type of health insurance plan that provides a network of healthcare providers much like a Health Maintenance Organization. PPOs got this name because they have lists of healthcare providers that they prefer you to use.
Will I need to file claims. The Periodical Payments Orders Working Party has been at the forefront of advising GI actuaries about the impacts on their work such as the need to use life insurance techniques in reserving. PPOs are a significant feature of insurers and reinsurers balance sheets already and are having an impact on pricing and capital modelling efforts of GI actuaries.
What is a PPO. A Preferred Provider Network or a PPO is a network of doctors hospitals and other health care providers who agree to provide health care at reduced rates to the members. PPO stands for preferred provider organization.
PPO Health Insurance Plans. A health maintenance organization HMO and a preferred provider organization PPO have several differences such as which doctors patients can see how much services cost and how medical records are kept. PPO stands for Preferred Provider Organization plan and with this plan type youll have the advantage of a lower deductible.
However visiting an out-of-network provider will include a higher fee and a separate deductible. Unlike an HMO PPO plans give participants the freedom to seek care from any in- or out-of-network provider. Given that theyre less restrictive than most other plan types they tend to have higher monthly premiums and sometimes require higher cost-sharing.
Just like an HMO or health maintenance organization a PPO plan offers a network of healthcare providers you can use for your medical care. 1 PPOs are a type of managed care health insurance plan like their distant cousins health maintenance organizations or HMOs. 1 PPO is short for Preferred Provider Organization and allows patients to choose any physician they wish either inside or outside of their network.
PPO stands for preferred provider organization. A PPO is a managed-care organization consisting of medical professionals and facilities such as primary and specialty physicians hospitals and other healthcare professionals. In addition your PPO insurance will pay if you see a non-network provider although it may be at a lower rate.
If you get your health care from these preferred providers you pay less. Theyre also sometimes called traditional plans because theyve been around longer than HDHPs have. Here are some key features.
But youll also pay more in monthly premiums.




/GettyImages-8972434181-b7ccb004f35c457b93a1701137183642.jpg)