For Prior Authorization Requirements training tools submission options and user guides click here. Non-Formulary Drug Prior Authorization Form Use this request form if the medication you want to request does not have an associated drug-specific form.
Https Www Healthchoiceaz Com Mdocs Posts Hca Pharmacy Services Prior Authorization Form Updated 102017 Hca Pharmacy Services Prior Authorization Form Updated 102017 5
Request form instructions Providers.
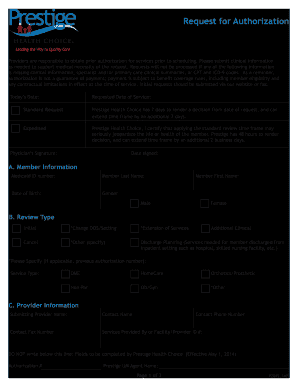
Health choice prior authorization form. KanCare Medicaid Behavioral Health PRTF Prior Authorization Request Form. Prior Authorization - Utah Department of Health Medicaid. Here are the ways your doctor can request approval.
The purpose of this form is to demonstrate medical justification for. Fax all completed Health Partners Medicaid and KidzPartners CHIP prior authorization request forms to 1-866-240-3712. Indiana Standard Prior Authorization Request Form for Health Care Services Please note.
Indiana Standard Prior Authorization Request Form for Health Care Services Opens in a new window. If any items on the Medica Prior Authorization list are submitted for payment without obtaining a prior authorization the related claim or claims will be denied as provider liability. 6 request prior authorization of a prescription drug.
The provider will have 60 days from the date of the claim denial to appeal and supply. Electronically through the issuers portal to request prior authorization of a health care service. 405 522-6205 option 6.
Coverage and Reimbursement Lookup Tool. Form can be faxed to. Submit by fax using the forms posted on the FutureScripts website.
Fill it out and fax it to us using the instructions provided on the form. If you are accessing the Electronic Prior Authorization form via the Internet Explorer browser please click here for a guide to ensure all documents are transmitted. If you are using a public or shared computer and you do not want to save your personal health information on that computer consider calling Member Services or print and mail the form.
Prior Authorization Request Form Medica requires that providers obtain prior authorization before rendering services. MA PET - PET CT Prior Authorization Form PDF Massachusetts Behavioral Health Prior Authorization Form PDF Massachusetts Transcranial Magnetic Stimulation Prior Authorization Form PDF Texas Standard Prior Authorization Request Form for Health Care Services PDF Vermont Uniform Medical Prior Authorization PDF. 4 request a guarantee of payment.
Use the Online Prior Authorization and Notification tool KanCare Medicaid Behavioral Health Inpatient Prior Authorization Request Form Opens in a new window. Prior authorization requests are reviewed by FutureScripts our independent pharmacy benefits manager on behalf of Independence. 800 522-0114 option 6.
Use the Online Prior Authorization and Notification tool KanCare Medicaid Behavioral Health Inpatient Prior Authorization Request Form. For Part D prior authorization forms please see the Medicare section. Step 2 Section A must be completed with.
UnitedHealthcare Prior Rx Authorization Form UnitedHealthcare prior authorization form. Or 7 request a referral to an out of network physician facility or other health care. Do not use this form to.
Authorized Representative Request PDF Medicare Member Authorization Appeal-appealing Medicare denials of medical prior authorization precertification requests PDF Medicare Non-contracted Provider Appeal Process PDF Medicare Appeals Provider Memo- Post Service PDF. Print and fax Open the form you wish to fill out. For all other services please reference the inpatient and outpatient requests to complete your request online or call 1.
To ensure that prior authorizations are reviewed promptly submit request with current clinical notes and relevant lab work. Medical Authorization Unit - for current status of requested services documentation requirements per type of requested service and the need for urgent authorization of services. A request form must be completed for all medications that require prior authorization.
The Fee For Service FFS Prior Authorization Request Form is to be completed by registered providers to request an authorization. Go to CoverMyMeds to submit a prior authorization request Call 1-800-555-CLIN 2546 Monday Friday 8 am. All mandatory fields on the form must be completed accurately in order to avoid delays in receipt and processing of.
For information on how to submit a preauthorization for frequently requested servicesprocedures for your patients with Humana commercial or Medicare coverage please use drop down below. 1 request an appeal. 5 ask whether a service requires prior authorization.
405 702-9080 local statewide 1-866-574-4991. Prior Authorizations Forms. Request prior authorization for Personal Care Attendant PCA Services What you need to know MassHealth Guidelines for Medical Necessity Determination Prior Authorization for Non-Pharmaceutical Services - Frequently Asked Questions Medical Necessity Review Forms MassHealth Drug List Prior Authorization Forms for Pharmacy Services.
Fax is not a secure method of transmission. 8 pm local time Fax a prior authorization request form to 1-877-486-2621. Providers should fax the completed FFS Prior Authorization Request Form as the coversheet for the supporting documentation they are submitting with the request.
Step 1 Enter todays date at the top of the page. Fax is not a secure method of transmission. Please include ALL pertinent clinical information with your Medical or Pharmacy Prior Authorization request submission.