PBMs vary in their organization and services because they originate from different types of businesses. The company constructs innovative solutions to meet the unique requirements and financial goals of their clients by allowing them to offer the.
 Pbm Transparency 50 State Network
Pbm Transparency 50 State Network
The organization operates as its business unit with a dedicated management team.

Pharmacy benefit management companies. Pharmacy benefit management companies PBMs operate between pharmaceutical manufacturers pharmacies patients and payers. Pharmacy Benefit Management PBM Market 2020-2027. The principal services offered by pharmacy benefit management companies PBMs are described.
The principal services offered by pharmacy benefit management companies PBMs are described. No Matter Your Mission Get The Right Benefits Management Tools To Accomplish It. Pharmacy benefits management companies PBMs design implement and administer outpatient drug benefit programs for employers managed care organizations and other third-party payers.
A PBM contracts with employers insurers and others to provide accessible and cost-effective benefits to those groups members. As a zero-spread full pass-through pharmacy benefit manager PBM Navitus aligns performance with plan sponsors benefit goals to deliver comprehensive clinical programs and costsaving strategies that lower drug trend and promote good member health. AscellaHealth provides customized and full-service pharmacy benefit management solutions and robust clinical programs.
Navitus Health Solutions LLC is a full service URAC-accredited pharmacy benefit management company. The IngenioRx and CVS partnership model has many. They use this position to influence access to and the cost of insurance coverage for drugs.
By aggregating lives covered under their many individual contracts with payers PBMs have formidable negotiating power. It is a combination of specialty pharmacy and mail order pharmacy coupled with pharmacy benefit management services. PBMs vary in their organization and services because they originate from different types of businesses.
PBMs manage or carve out prescription drug benefits independently of other health care services such as physician and hospital services. Over the past decade pharmaceutical benefit management companies PBMs have assumed an expanded role as intermediaries in the design and administration of pharmacy programmes. By aggregating lives covered under their many individual contracts with payers PBMs have formidable negotiating power.
Pharmacy benefit managers may be able to get deeper discounts from drug manufacturers if the drug companies can keep the size of the discounts secret and not have to offer them to every other PBM. ProCare RX is national pharmacy benefit manager with decades of experience in healthcare information technology. No Matter Your Mission Get The Right Benefits Management Tools To Accomplish It.
Pharmacy benefit managers or PBMs are companies that manage prescription drug benefits on behalf of health insurers Medicare Part D drug plans large employers and other payers. PBMs now provide a range of sophisticated clinically oriented services that increasingly influence physicians prescribing patterns and patients access to pharmaceuticals. In the beginningPBMs were put in place to create convenience.
Top Companies Express Scripts Holding Company UnitedHealth Group Inc Magellan Health Inc. Advertentie Review the Best Benefits Management Tools for 2021. Save Time Money - Start Now.
Pharmacy benefit management companies PBMs perform functions in the US market-based healthcare system that may be performed by public agencies or quasi-public institutions in other nations. A PBM contracts with employers insurers and others to provide accessible and cost-effective benefits to those groups members. 04-07-2020 0114 PM CET IT New Media Software.
By negotiating with drug manufacturers and pharmacies to control drug spending PBMs have a significant behind-the-scenes impact in determining total drug costs for. Pharmacy benefits managers are third-party administrators of prescription drug programs who contract with employers insurers and pharmacies to manage prescription drug coverage for pharmacy patients. Save Time Money - Start Now.
Advertentie Review the Best Benefits Management Tools for 2021. The healthcare system is very complex with many companies involved that go far beyond the doctor and pharmacist relationship.
What Is A Pbm Enabling Healthy Decisions
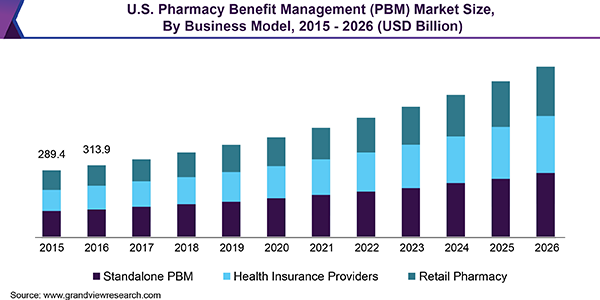 U S Pharmacy Benefit Management Market Report 2019 2026
U S Pharmacy Benefit Management Market Report 2019 2026
 Figure 1 From Pharmacy Benefit Management Companies Pbms Semantic Scholar
Figure 1 From Pharmacy Benefit Management Companies Pbms Semantic Scholar
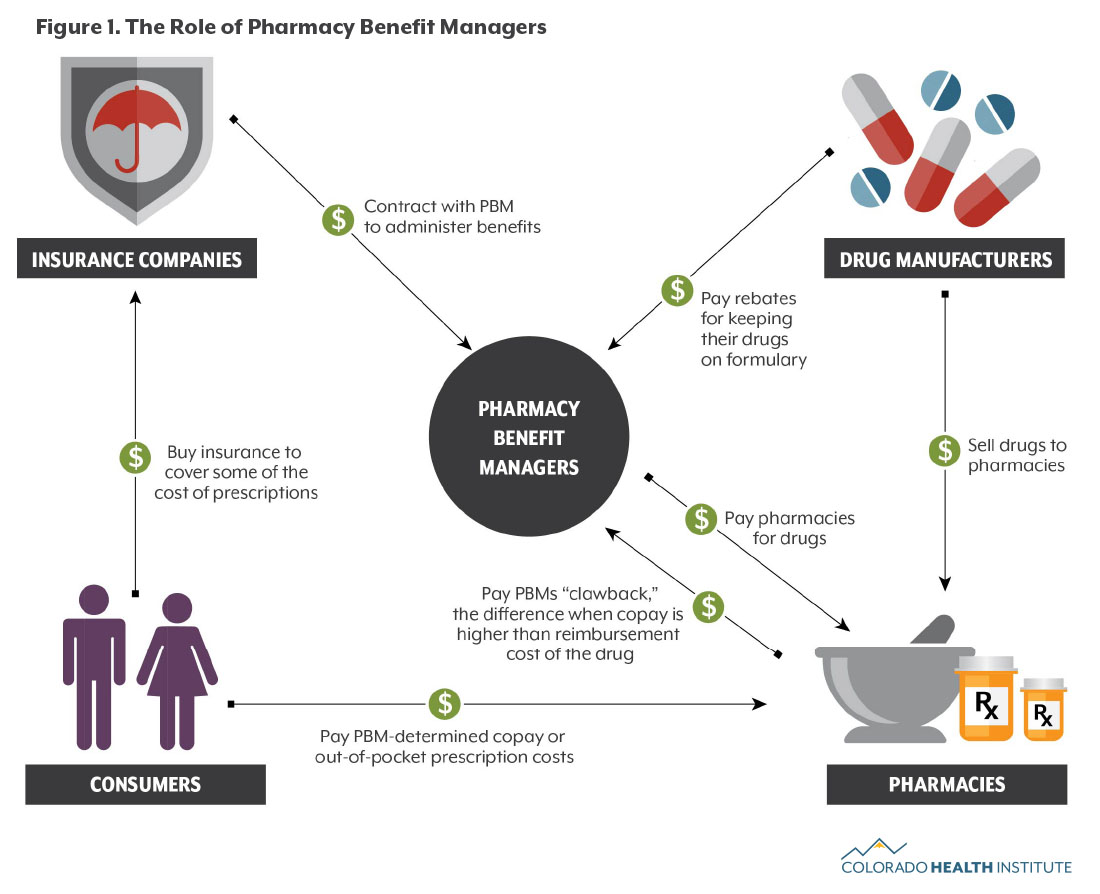 Understanding Pharmacy Benefit Managers Colorado Health Institute
Understanding Pharmacy Benefit Managers Colorado Health Institute
 Drug Channels Cvs Express Scripts And The Evolution Of The Pbm Business Model
Drug Channels Cvs Express Scripts And The Evolution Of The Pbm Business Model
 Pharmacy Benefit Managers Help Companies Cut Costs
Pharmacy Benefit Managers Help Companies Cut Costs
 The Relationship Between Pharmacy Benefit Managers Pbms And The Cost Of Therapies In The Us Pharmaceutical Market A Policy Primer For Clinicians Sciencedirect
The Relationship Between Pharmacy Benefit Managers Pbms And The Cost Of Therapies In The Us Pharmaceutical Market A Policy Primer For Clinicians Sciencedirect
 Drug Channels Cvs Express Scripts And The Evolution Of The Pbm Business Model
Drug Channels Cvs Express Scripts And The Evolution Of The Pbm Business Model
Pharmacy Benefit Management Industry Definition
:max_bytes(150000):strip_icc()/largest-pharmacy-benefit-managers-2663840-FINAL-5be9a0b746e0fb0026ca5bd6.png) How Pharmacy Benefit Managers Pbms Work
How Pharmacy Benefit Managers Pbms Work
 Pharmacy Benefit Managers And Their Role In Drug Spending Commonwealth Fund
Pharmacy Benefit Managers And Their Role In Drug Spending Commonwealth Fund
 Pharmacy Benefit Managers Practices Controversies What Lies Ahead Commonwealth Fund
Pharmacy Benefit Managers Practices Controversies What Lies Ahead Commonwealth Fund
Pharmacy Benefit Management Industry Definition
 Drug Channels Follow The Dollar Math How Much Do Pharmacies Wholesalers And Pbms Make From A Prescription
Drug Channels Follow The Dollar Math How Much Do Pharmacies Wholesalers And Pbms Make From A Prescription

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.