Prior Authorization Criteria Health Alliance Plan 2021 Date Effective. In most cases the prescription drugs you get in a.
Https Www Bcbsal Org Pdfs Egwp S1030 Pda Egw 13 Wb Pdf
Huskamp HA1 Stevenson DG Donohue JM Newhouse JP Keating NL.
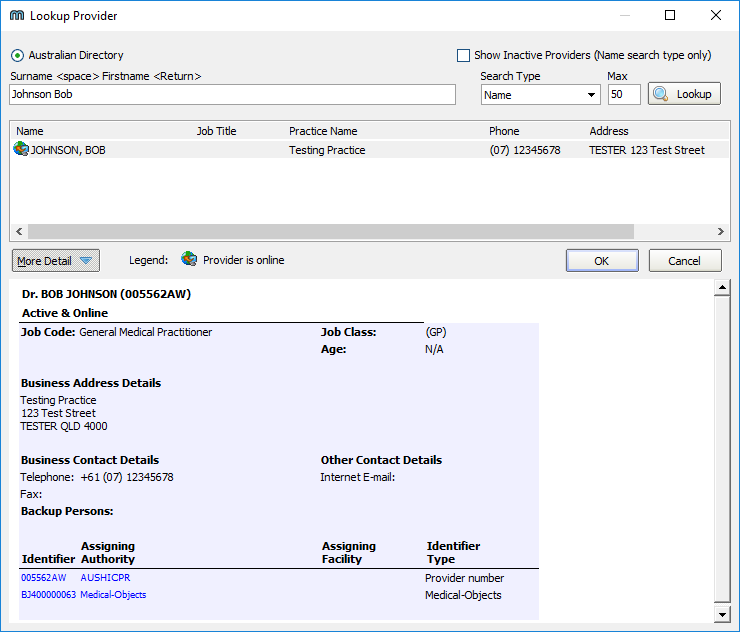
Medicare part d prior authorization. Other user management restrictions include Quantity Limits and Step Therapy. This form is available both in English and Spanish. Medicare Part D Coverage Determination Request Form PDF 38751 KB For certain requests youll also need a supporting statement from your doctor.
Box 25183 Santa Ana CA 92799. Part D plans as defined in 42 CFR 4234 include Prescription Drug Plans PDPs and Medicare. Under this final rule Part D plan sponsors will be required to support version 2017071 of the National Council for Prescription Drug Programs NCPDP SCRIPT standard for four electronic Prior Authorization ePA transactions and prescribers will be required to use that standard when performing ePA transactions for Part D-covered drugs they wish to prescribe to Part D-eligible individuals.
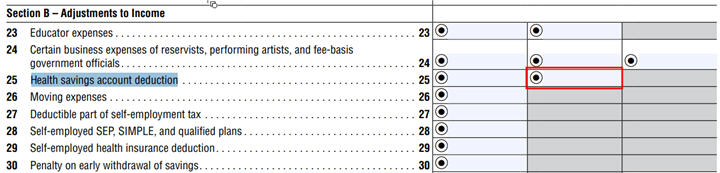
Formulary ID 21478 Version 6 Updated 4012021 1 Medicare Part D drugs with prior authorization criteria Employer-based plans Prior Authorization Group ACTHAR Drug Names ACTHAR PA Indication Indicator All Medically -accepted Indications Off-label Uses-. PT Saturday If you cannot submit requests to the OptumRx PA department through ePA or telephone click here. Under Prior Authorization benefits are only paid if the medical care has been pre-approved by Medicare.
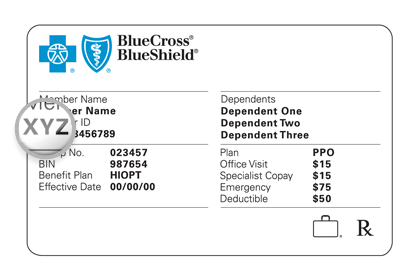
However some plans require an additional monthly premium for drug coverage. Get forms in alternate formats. Part D vaccine coverage.
To get the Medicare form you need find the situation that applies to you. The Medicare Prior Rx Authorization Form or Drug Determination Request Form is used in situations where a patients prescription is denied at the pharmacy. Private for-profit plans often require Prior Authorization.
Medically accepted indications are defined by CMS as those uses of a covered Part D drug that are approved under the Federal Food Drug and Cosmetic Act or the use of which is supported by one or more citations included or approved for inclusion in any of the compendia described in section 1927g1Bi of the act. 1Department of Health Care Policy Harvard Medical School and Division of General Internal Medicine Brigham and Womens Hospital Boston MA 02115 USA. Use these documents to view the lists of drugs that have prior authorization or step therapy requirements and the rules that apply to each drug.
Once a patient or their physician receives a written denial coverage determination they should submit a coverage determination request form asking for the drug. Fill out Authorization to Disclose Personal Health Information. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification.
Prior Authorization is one of the usage management tools available to a Medicare Part D plan to help control drug usage and reduce plan costs. Other ways to submit a prior authorization Having difficulties with ePA. I want to make sure Medicare can give my personal health information to someone other than me Authorization to Disclose Personal Health Information formCMS-10106.
Prior Authorization is about cost-savings not care. Coverage and prior authorization of psychotropic drugs under Medicare Part D. The Request for Reconsideration of Medicare Prescription Drug Denial model notice has been updated to include C2Cs contact information as they are the Part D QIC effective 020121.
Request for Administrative Law Judge ALJ Hearing or Review of Dismissal. Members of Medicare Advantage MA Plans typically receive Part D coverage automatically. PT Monday-Friday and 6 am.
Call 1-800-711-4555 5 am. 05012021 Formulary ID 21357 V12 17 AYVAKIT Products Affected Ayvakit PA Criteria Criteria Details Exclusion Criteria NA Required Medical Information Diagnosis prior therapy used result of prior therapy. Except for vaccines covered under Medicare Part B Medical Insurance Medicare drug plans must cover all commercially available vaccines like the shingles vaccine when medically necessary to prevent illness.
Prior authorization is a requirement that a health care provider obtain approval from Medicare to provide a given service. You can submit a verbal PA request. The Centers for Medicare and Medicaid CMS defines Prior Authorization as.
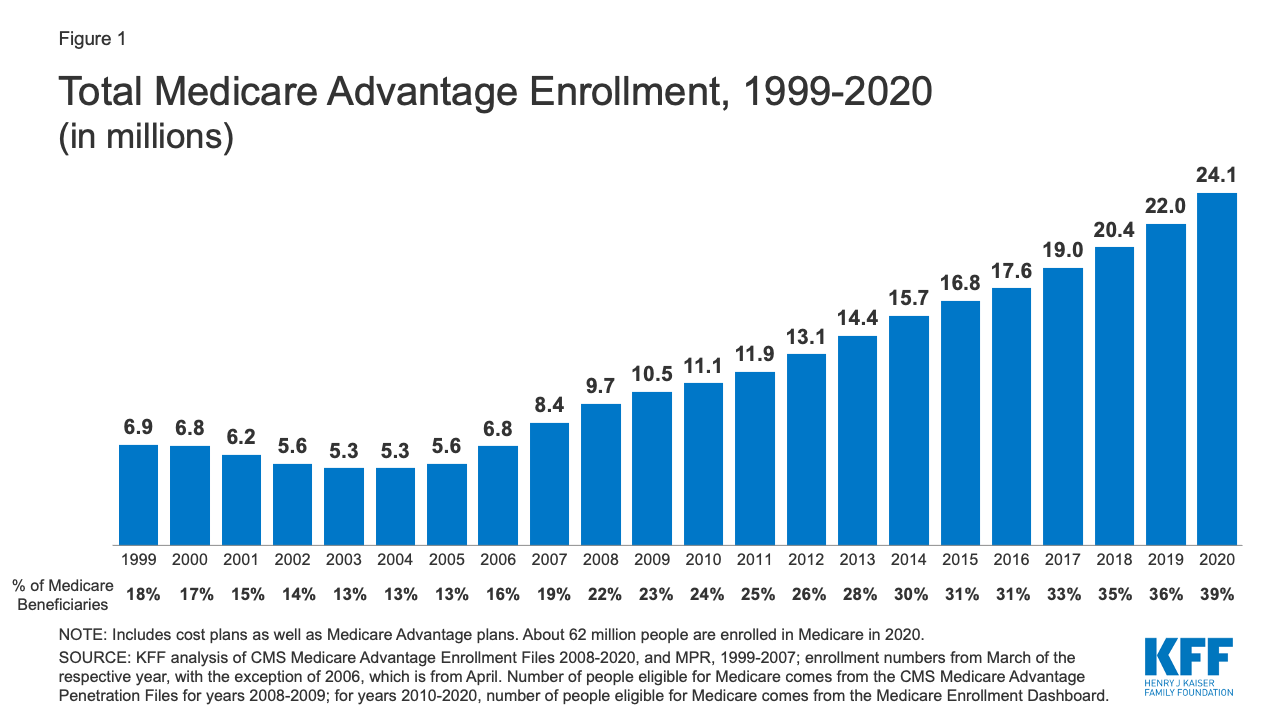
Medicare Advantage MA plans also often require prior. As part of the Calendar Year 2021 Outpatient Prospective Payment SystemAmbulatory Surgical Center Final Rule CMS-1736-FC CMS is adding Implanted Spinal Neurostimulators and Cervical Fusion with Disc Removal to the nationwide prior authorization process for hospital outpatient department OPD services effective July 1 2021. OptumRx Prior Authorization Department PO.
If you wish to request a Medicare Part Determination Prior Authorization or Exception request please see your plans website for the appropriate form and instructions on how to submit your request. Contact CVS Caremark Prior Authorization Department Medicare Part D. Drugs you get in hospital outpatient settings.
Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. This document explains certain changes in Medicare policies to help Medicare Part D patients use opioid medications more safely.