Heres an example of step therapy. For example if Step 1 and Step 2 drugs both treat your medical condition we may not cover the Step 2 drug.
 Cms Medicare Advantage Plans Can Require Step Therapy Medpage Today
Cms Medicare Advantage Plans Can Require Step Therapy Medpage Today
Step therapy may sound like an exercise program but it actually refers to managed care for prescription drug therapies and a process that healthcare insurers use to control prescription drugs costs.
Step therapy medicare. 2021 Step Therapy List for Medicare Part B Drugs Acromegaly Drugs. HCPCS codes Generic name Trade name Step therapy requirement Prior authorization requirement effective date. For consumers the Centers for Medicare Medicaid Services CMS website defines step therapy as follows.
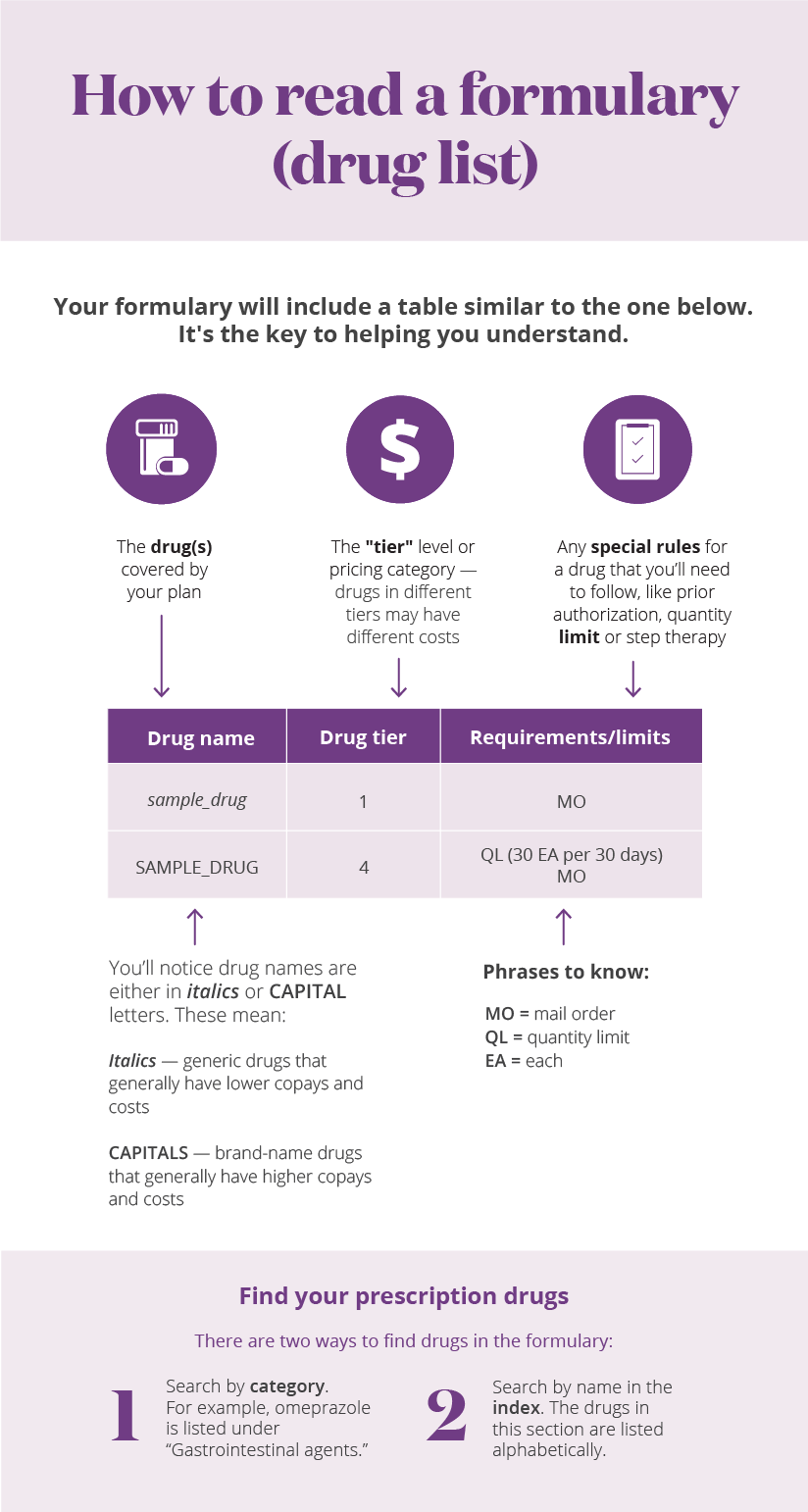
Medications that may typically be included as a part of step therapy are drugs used to treat the most common medical conditions such as. You take a generic drug to lower your cholesterol but its not working. We have an exception process in place for drugs with prior authorization step therapy or other requirements or limits on coverage.
Step therapy or other utilization management policies may not be used as an unreasonable means to deny coverage of medically necessary services or to eliminate access to a Part B covered benefit. What is Step Therapy. Drugs That Require Step Therapy ST In some cases Express Scripts Medicare PDP requires you to first try certain drugs to treat your medical condition before we will cover another drug for that condition.
CMS is also finalizing regulations under which Medicare Advantage MA plans can implement step therapy for Part B drugs for new patients. Medicare Part B Step Therapy Drug List HCPCS Code Medication Name Requirement Effective Date J2786 Cinqair reslizumab injection Step Therapy 010119 J0517 Fasenra benralizumab injection Step Therapy 120119 J2182 Nucala mepolizumab injection Step Therapy 010119 J2357 Xolair omalizumab injection Step Therapy 010119. Step therapy is sometimes referred to as a fail first protocol in that the lower-cost medication has to fail to treat a patients condition before the insurer will pay for higher-cost drug therapy.
This document lists the medical benefit drugs that have authorization or step therapy requirements for Medicare Advantage members. But its more expensive. Your doctor prescribes a different medication that works well.
Step therapy is a type of prior authorizationIn most cases you must first try a certain less expensive drug on the plans formulary thats been proven effective for most people with your condition before you can move up a step to a more expensive drug. Colony Stimulating Factors Short. To check if prior authorization or step therapy applies search one of our online drug lists.
Colony Stimulating Factors Long Acting. This document contains the Step Therapy protocols for Medicare Part B drugs that are associated with the Independent Health Medicare Advantage Plans mentioned above. In most cases you must first try a less expensive drug on the Medicare Prescription Drug Plans formulary also called a drug list that has been proven effective for most people with your condition before you can move up a step to a more expensive drug.
Your doctor prescribes another medication but its still not working. See the revision history at the end of this document for information about changes to this list. These drugs require prior authorization only when used for oncology to treat cancer.
Step therapy approaches must be approved by the plans pharmacy and therapeutics committee and when patients appeal a denial of a drug the plans decision-making timeframe will be shorter than it is currently and will mirror Part D rules. Medicare B Step Therapy Policy Drugs that require Prior AuthorizationStep Therapy are indicated on our drug list. Allergies Asthma COPD Cardiovascular health Diabetes High cholesterol Mental health issues Bladder problems Acid reflux and heartburn.
If you have a formulary drug subject to Step Therapy you are required to try a less-expensive medication before the drug plan will pay for the formulary drug that your doctor may have originally prescribed. Step therapy is a type of prior authorization for drugs that begins medication for a medical condition with the most preferred drug therapy and progresses to other therapies only if necessary promoting better clinical decisions. You find out that it.
Your doctor must prescribe a less expensive step-one drug such as over-the-counter or generic medications first. Step Therapy is a utilization management restriction that your Medicare Part D prescription drug plan can add to a formulary medication. Step therapy is also known as step protocol or a fail first requirement.
If it doesnt work ie it fails then your insurance will consider covering a costlier drug like a lower-cost brand-name medicine. Are plans required to review all National Coverage Determinations NCDs. One of these special requirements or coverage limits is known as step therapy where we require a trial of a preferred drug to treat a medical condition before covering another non-preferred drug.
Step therapy is a type of prior authorization. If you have any questions please contact our Medicare Member Services Department at. Step therapy also known as fail first is a form of prior authorization.
Tim Hale Photography Getty Images. This is dependent on the therapy described to treat your medical condition.